
[Skip to the quiz if you’d like]
On his way over to Charlie’s, Bill connected with Reggie Hammond, his neighbor from across the street. Reggie and his wife Felicia were in their front yard surveying the scene. They were both OK, and their house had minimal damage. There were some broken windows and missing roof shingles, but that looked to be about it. Reggie accompanied Bill to Charlie’s, as it looked like something bad happened.
A 70-foot poplar tree dissected Charlie’s house diagonally from the front yard to the back. It did not look good. The brick walls of the house looked like folded paper where the tree impacted it.
“Charlie, where are you guys?” Bill yelled to his friend.
“In the back.” Was the muffled reply from Charlie.
The two men snaked their way through a crevasse of brick, wood, and tree into Charlie’s house. They were in the living room and could see that the tree had crushed the wall between it and the family room in back. They saw Charlie with his back to them to their left, but could not see Charlie’s wife, Eileen.
“Charlie, Reggie Hammond and I are right behind you. Don’t turn around. Keep your head straight and keep looking forward.” Bill said.
“OK. I can’t get up. My leg is under the tree. Eileen isn’t talking. She won’t wake up. She’s breathing funny.” Charlie sounded panicked, frustrated and scared.
“OK Charlie, we’ll get to her in just a second.” Bill replied.
As he and Reggie climbed over the debris that was once a wall and into the family room, Bill deduced that Charlie and Eileen had been sitting on the couch that was against the wall that was now gone. It looked like the tree had fallen in between them, knocking Eileen across the room and pinning Charlie to the floor by his lower right leg.
“Reggie, can you look over Charlie while I go check on Eileen?” asked Bill.
“Sure thing.” Reggie said.
“What hurts Charlie?” Reggie asked.
“My damned leg, Reggie. I can’t get it out. I’m fine otherwise. Didn’t get knocked out. Didn’t hit my head. I’m fine. You’re better off helping out Eileen.” Said Charlie.
“OK Charlie, I understand. Let me check your pulses and get a good look at that leg. I just want to make sure you’re not bleeding out somewhere and we don’t know it.” Reggie said.
Charlie nodded impatiently and Reggie got about his work.
Bill stepped over the tree, took one look at Eileen, and swallowed hard. She was on her right side with a very large deformity to the left side of her head. As he got closer to her, he saw that her eyes did not register his presence. He shone his Surefire G2 flashlight in them and saw that her left pupil was totally dilated and her right pupil was on its way to the same. Neither of them constricted with the light. Eileen’s breathing was off. She would breath deeply for a few seconds, then stop completely for a few seconds, and repeat the cycle.
“Biot’s respirations.” Bill thought to himself. This breathing pattern can show up when a person has a brain injury or bleed severe enough to cause the brain to herniate through the large hole in the skull, the foramen magnum, where the brain and spinal cord connect and the cord is enveloped by the vertebrae. Bill started to suspect that the blunt trauma to the side of Eileen’s head caused a bad bleed inside of her skull.
He reached down to take Eileen’s radial pulse on her left wrist and noticed that her arms were extended out but her wrists were flexed. Then he noticed that her legs looked the same with the toes pointed down. He remembered it was called decerebrate posturing, and it was another sign of a very serious brain injury. As he felt her wrist, the pulses were very slow, but the strongest he ever felt. He pinched the web of flesh between her left thumb and index finger hard.
Nothing.
He pinched harder.
Still nothing.
Without immediate evacuation to surgical care, Eileen was dead. “Hang in there, Eileen. This is gonna be hard.” Bill whispered into his neighbor’s ear.
Bill stiffened his back and said slowly and loudly, “Charlie, Eileen is not well. She needs a lot of help right now. Are you OK if we get her out of here before you?”
“Oh God, please. Yes. I can’t lose her.” Charlie replied. His voice cracked.
“OK buddy. Let me see what I can do.” Said Bill.
Bill did not have any of the things he needed to help get Eileen prepared for transport. He did have a ventilator bag in his medical kit, but no supplemental oxygen. He could try hyperventilating her with room air to see if that helped the herniation. At this point, there wasn’t a whole lot he could do, but he had to try.
He called Reggie over to help. The fact that it was Reggie Hammond of all people was a stroke of very good luck. Reggie was a retired senior chief engineman from the Coast Guard and there was very little that would rattle him. He was kind and quiet, but was able to flip a switch and slip right into business mode when needed. When “The Senior” tapped you on the shoulder, you got into gear.
Bill looked at his neighbor and said, “Reggie, we need to try and help her breathe better. I’m going to need you to help me with this and then run the ventilator so I can get on the radio and see if we can get her out of here.”
“Not a problem boss, let’s do this.” Reggie replied.
Bill placed a King LT-D airway. It is a blind insertion airway device that doesn’t require a laryngoscope and is ideal for people who don’t place advanced airways regularly. It is a supraglottic airway that uses two air bladders to seal off the esophagus and isolate the trachea as well as anchor itself in the oropharynx, allowing a patient to be ventilated with a bag-valve mask. Bill carried these in his kit because they had become standard equipment in prehospital medicine and were easy to use. He confirmed its placement by listening to Eileen’s lungs with his stethoscope while Reggie squeezed the ventilator. Reggie continued to ventilate and was helping Eileen breathe at twenty breaths per minute.
Bill switched over to the ARES frequency he was on earlier and stood by for almost a minute. The air was clear.
Bill opened. “This is KXXXX at station Patrick Henry with an emergency communication. Do you copy?”
The radio crackled back. “Receiving. What is your emergency? KXXXX?”
“I need immediate medical evacuation for one unresponsive patient with a severe head trauma.” Said Bill.
There was a pause for ten seconds. “Received. Stand by KXXXX.”
Bill waited. Almost two minutes went by. The radio came back to life.
“KXXXX. Ground transportation will not be available in your area for at least 48 hours. Air transportation will be online in two hours. The regional Level I trauma center is down. A mobile emergency department is being set up in the parking lot of the football stadium in Lumberton. We can only send helicopters by greatest need and greatest number. I need a census within two hours of total number of patients triaged in red, yellow, green, and black as well as missing. Stay on this frequency and report in at 1705 hours. Coordinator out.”

Bill signed off, “KXXXX at station Patrick Henry copies.” He hung his head, closed his eyes, and heaved a sigh.
Bill looked at Charlie. His eyes were locked onto the ceiling as they filled with tears and his chin trembled.
“Can you bring her over to me?” whispered Charlie.
“But Charlie, we…” Bill started to say.
“Dammit, just bring her over to me! And take that thing out of her mouth! I heard what the man said on the radio. I know what’s going on. Let me be with her. Let me hold her.”
Bill looked over to Reggie, who was still tending to Eileen. Reggie nodded, and Bill went into the other room and grabbed a sheet. Reggie stopped the ventilations and removed the airway. They got her on the sheet and laid her next to Charlie.
Charlie cradled her to his chest with his left arm and began to sob in anguish, his face contorted in pain, “It’s OK baby. It’s OK. I’m here. You’re OK now.”
“Charlie, we need to get you out…” said Bill
Charlie interrupted, “Just leave us! Please. Come back later.”
At this point, Bill looked up at Reggie, whose gaze was fixed onto him like a tiger about to jump onto a deer. Reggie made an infamous “knife hand” motion towards the hole they came in and punctuated it with a nod in the same direction without ever breaking eye contact.
The two men got outside of Charlie’s house and Reggie turned to Bill.
“Bill, I know Charlie is your friend. He is my neighbor, too. This is painful. This is horrible. This is almost unbelievable. But right now, he’s a yellow and Eileen is a black. That’s two that we know about.
“The reality is, we need to get him out of there. We need to get people going through this neighborhood and finding anyone else that needs help. We need to get people organized and moving to make this thing suck less than it already does. And that means you, me, and everyone else with a pair of stones needs to push that sadness back down and get on it, NOW.
“I’m going to go over there and I am going to get people organized for search and rescue. I will get some people to come over here and help you get Bill out and Eileen taken care of. I’ll go talk to Felicia and have her set up a treatment area in our garage, since our house is in good shape.
We need to get on this, because in two hours, we have an opportunity to let people who can help us know how much help we need. From what the man said on the radio, this is a no-shitter, and this is just beginning.
You’ve done good today. Your wife and family are safe. You’ve helped your friends. Now we need to prepare a whole bunch of people for something they’ve never experienced before, and we need to keep as many people alive as we can.”
With that, Reggie pulled a cigar case out of his front shirt pocket, took out a Romeo y Julieta Belicoso, jammed it into the right side of his mouth, bit down on it, and straightened his cap. He squared himself towards Bill, stuck his chest out, put a firm right hand on Bill’s left shoulder and gave it a good squeeze.
He looked Bill straight in the eye and winked while saying, “It’s time to go to work.”
With that, Reggie jogged off towards Felicia and started waving people in his direction.
Bill stared at the ground and thought of his friend with his dying wife inside the house. Bill thought of his own wife and he started to heave and sob. After a minute, he gritted his teeth and inhaled deeply.
“Keep going,” he said to himself, “you’ve got to keep going.”
***********************************************************************************************************************
In the previous post, we knocked out the first part of the rapid trauma assessment that allowed us to establish a patient treatment priority. Buckle your seatbelts, because the rest of the assessment is long, but fast. If you were fast with the first part of the assessment, you have eight and one half minutes left. If you were slow, you have seven minutes left.
We’re going to do a more detailed assessment if we have the time and the patient is stable enough. The rough analog to this in TCCC would be the Tactical Field Care phase or the CASEVAC phase depending on the situation. We want to get a better – still rapid – look at the patient and find more things to fix if they are life threats. Key point here – TAKE HIS CLOTHES OFF. Seriously. If you can’t see it, you can’t find it, and you won’t fix it. I usually keep my patient’s underoos on if they are 100% conscious, alert, and oriented and inspect “down there” with their permission after a description of what I need to look for and why. If their mentation is altered, the underoos are coming off so I can check the genitalia and rectum for bleeding if there is any thoracic /abdominal trauma or pain in any area that indicates thoracic /abdominal injury.
Head, eyes, ears, nose, and throat (HEENT)
Start at the head and work your way down. Inspect and palpate – which means feel around in vulgar terms – the head and neck. Remember the DCAP-BTLS mnemonic. Key to look out for is fluid coming out of the ears or nose, as it could be cerebral spinal fluid (CSF), which indicates a skull fracture of some kind or disruption of the blood / brain barrier. If you see it, dab it with a gauze 2×2 or 4×4. If it looks like a pink blood spot with a halo around it, that’s CSF.

CSF on gauze. Notice the halo.
Source: http://medicinexplained.blogspot.com/2011/12/csf-rhinorrhea-double-ring-sign-ring.html
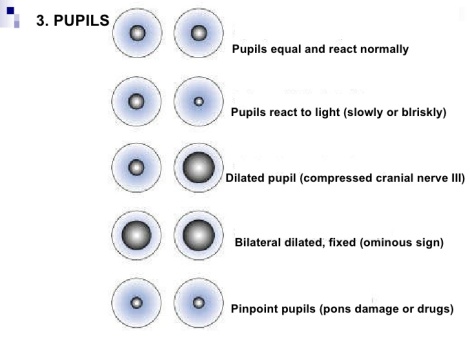
If you feel bones grinding around – known as crepitus – this is bad, too, as it also indicates skull fracture. Check the pupils and eyeballs. Are they equal, round, and responsive to light? Great. If one or both are dilated and your patient has an altered mental status, you are in deep because your patient probably has a bleed going in his brain. The contents of the skull are roughly 80% brain, 10% CSF, and 10% blood. Since the skull is a fixed volume, if anything new shows up in there or the amount of blood shoots way up, all sorts of issues with cerebral perfusion pressure (CPP) will occur because of increased intracranial pressure (ICP) [Recommended: Look up the Monroe-Kellie hypothesis and autoregulation.] If you are out in the middle of nowhere without rapid evacuation to an OR, this is most likely fatal, as was Eileen’s case above.
Clinical note: Another thing about Eileen’s case. A head injury with brain herniation will most likely present with projectile vomiting as the herniation progresses. I didn’t put that in the scenario because I’m lazy, but it’s a good bet that someone in her condition would be vomiting, thus complicating the situation even more. Eileen is presenting with irregular respirations (Cheyne-Stokes, Biot’s, ataxic, etc.) and implied severe hypertension (systolic greater than 180mmHg and diastolic greater than 120mmHg) and bradycardia (heart rate less than 60 beats per minute) from Bill’s radial pulse check, which are known clinically as Cushing’s Triad in patients suspected of increased intracranial pressure or brain injury.
Look for anything in the mouth that can result in an airway threat and take steps to mitigate. Teeth, Copenhagen, soft tissue, etc. The tongue is the most common airway obstruction, and if you hear snoring noises from your patient, most likely his tongue is in the back of his throat. Try basic airway maneuvers to open the airway like the head-tilt chin lift or modified jaw thrust first, and an oropharyngeal airway (OPA) adjunct if the patient has no gag reflex, and a nasopharyngeal airway adjunct (NPA) if he does have a gag reflex. Here’s a nice instructional video for measuring and placing OPAs and NPAs.
If cervical spine injury is suspected, stabilize c-spine and apply a c-collar if available. Inspect and palpate the back of the neck for crepitus or deformity before applying the c-collar. If you don’t have one, use a SAM splint, towels, clothing, and tape to create a hasty c-collar. The goal is to prevent the head from moving around and exacerbating a cervical vertebrae fracture that could slice into the spinal cord. Make sure you’re not restricting circulation in the neck or breathing with the hasty c-collar.

Improvised c-collar. Dig it.
Source: http://www.trailspace.com/forums/trip-reports/topics/130492.html
Neck
Inspect and palpate the neck. Look for any bruising or open wounds on the neck. If there is a wound near the jugular vein or carotid artery, apply an occlusive dressing like Vaseline gauze, or plastic wrap (a section of MRE rapper, etc.) to prevent air from going into the wound and causing an air embolus in the circulatory system. You may need to position the patient on his left side to mitigate the air embolus from entering the heart. Keep c-spine precautions in place if you do.
If the jugular veins are distended (bulging out), this could be a sign of circulatory compromise, with the right side of the heart failing to move blood adequately. This could be from a pericardial tamponade, which can only be fixed in the hospital, a tension pneumothorax or even a severe hemothorax.
Jugular venous distension. Never fun to see in trauma.
Source: http://commons.wikimedia.org/wiki/File:Jugular_Venous_Distention_%28JVD%29.JPG
If the patient’s windpipe – i.e. trachea – is deviating to one side, this is an ominous sign of a late stage tension pneumothorax, also known as a collapsed lung.

Tracheal deviation in a tension pneumothorax.
Source: http://blog.tacmedsolutions.com/?p=86
You may need to needle decompress the affected lung, but you’ll need to assess the chest to make the call.
Chest
Check the upper chest for little bumps. If you can push down on them and they pop like Rice Krispies, this is probably subcutaneous emphysema, and is a sign that the patient’s airway has been compromised. The larynx, trachea or bronchi may have been damaged and air leaking air into the chest cavity. Look for this sign in pneumothorax as well. Personally, I have never seen this in the field, but Doc Grouch has seen it in his work, and in his words “It is unmistakable, if you have felt it once, you never forget, and really you can’t miss it.”
The other critical findings for a tension pneumo are low blood pressure, tachycardia (pulse > 100 bpm), a narrow pulse pressure (this is the difference between the systolic and diastolic pressures. A normal pulse pressure is 120/80. A narrow pulse pressure with hypotension is 70/60), absent lung sounds on the affected side, fast, shallow breathing, and low O2 saturation. The trachea will deviate AWAY from the side of the collapsed lung. NOTE: Tracheal deviation is a LATE sign in a tension pneumo. Look for the other signs and symptoms first. If you wait for tracheal deviation to show up, you’ve probably killed your patient.
You’ll need a 3.25” 14 gauge need and catheter for decompression. Insert the needle in the second intercostal space just above the third rib at the midclavicular line (in line with the middle of the collar bone) of the affected side. Press hard and remove the needle, and if you do it correctly, you’ll hear a flood of air come out of the catheter. Create a flutter valve with a spare glove fingertip and place it over the top of the catheter. Some of the newer catheters have a one-way valve built in, so what you have already may be adequate.
The 3.25″ needle is preferred, because most likely your tribe is full of studmuffins with 50″ chests who all bench 550lbs easily. The other guys have all the fat dudes with man tits. In either case, that’s a lot of material between the skin and the chest cavity full of air. The shorter needles may not make it all the way through, so keep that in mind.
TCCC Note: The threshold for chest decompression is much lower in TCCC. If your patient has a chest injury and is having trouble breathing, you decompress him. Why? Because if there are bullets flying and decompressing his chest allows you to put an M4 back in his hands and fire back, then you do it. Please DO NOT use the TCCC threshold in a non bullets flying scenario. If you have time, use it and be sure in your diagnosis before performing an advanced procedure.
Press on the clavicles for crepitus. If it is present, note it but keep going. Unless the clavicle is so screwed up that it looks like it is stabbing the the lungs, or you see sign of massive hemorrhage from a nick of subclavian artery and/or vein, it is probably not a life threat.
Press down on the ribs and feel for crepitus. Notice the patient’s work of breathing. Are both sides of his chest rising and falling in unison? That’s good. If you feel crepitus and see a portion of the ribs moving collapsing while the rest of the ribs expand and vice versa, your patient may have a flail segment, which is a section of ribs that have broken completely away from the rib cage. This is a serious sign and should be fixed when found. You want to tape down a folded shirt, saline bag, or bulky dressing over the wound site. Tape it down tightly, because you’re trying to prevent the flail segment for engaging in the paradoxical movement that can compromise breathing. Be highly suspect of a pneumothorax / hemothorax if you see this. This video shows it pretty well. Look how much effort this guy is putting into breathing. If he doesn’t get help soon, he’s going to tire out, crap out, and you’re going to need resources to breathe for him.
If you find puncture wounds over the chest, then cover them with occlusive dressings like Vaseline gauze, plastic wrap, or some of the fancy chest seals like the Asherman, Halo, Hyfin, and Bolin. If you are using Vaseline gauze or plastic wrap, tape it down on three sides only and leave one side open to allow for burping the wound.

Vaseline gauze. Cheap and effective.
Clinical note: I list Vaseline Gauze as a cheap alternative to the fancier chest seals. Honestly, the best thing to do with it is to open the mylar wrapper carefully, pull out the gauze, use it for kindling or something, and use the wrapper as the chest seal. Personally, I like the Hyfins, they’re big.
If the wound is gurgling, then you very likely have a pneumo / hemothorax to deal with. Make sure to count all of the puncture wounds and their locations. If you can, roll the patient on his side and assess the back for wounds and injuries. If there are more holes in the chest / thorax area, count them, note their locations, and get occlusive dressings on them. Don’t worry about exit or entry classifications. What matters is the number of holes in your patient’s body and what the implications are for what’s happening inside where you can’t see.
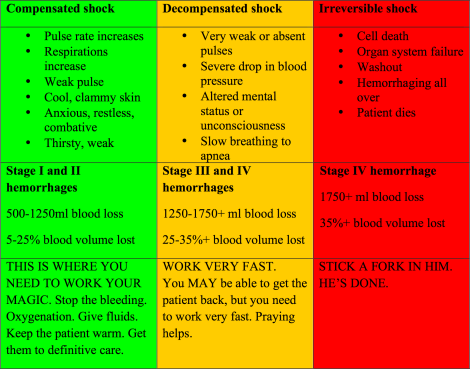
A quick talk about hemothorax and fluid in the lungs. A hemothorax is blood filling up the space in the chest that once was filled by your now collapsing lung. The space in your chest is big enough to hold 25-40% of your blood supply. Remember the shock table.
25% of blood volume and above is Stage III and Stage IV hemorrhages. Like a pneumothorax, the blood in the chest cavity prevents the lung from fully inflating, but is less likely to result in the same amount of tension as a tension pneumothorax. Needle decompression will not be an effective treatment for a hemothorax. A chest tube placed on the midaxillary line (think inline with your armpit) in the fifth intercostal space in the ribcage is going to be a better solution in getting the blood out. This is not something that you see done in a prehospital setting very often, but if you have the training and equipment to do it, knock yourself out. If you know you have a hemothorax in the field and your patient is dying from it, you may need to place your decompression needle in the fifth intercostal while the patient is supine and try to get some of the blood out. If you are having to do this, your day is very, very bad. Groovy video of chest tube insertion below. Watch the whole thing if you have time. Skip to 6:20 if you don’t.
Fluid in the lungs is just that. It can be water, blood, vomit, beer, you name it. The fluid fills the alveoli and prevents O2 and CO2 from exchanging at the capillary membrane. Get enough fluid in your lungs and you will not be able to exchange enough gas to stay alive and will die quickly. The alveoli lose their surfactant and collapse, making it impossible for them to continue to hold and exchange air. This condition is called atelectasis and it is very bad. People who survive drownings can have this happen to them days after they are rescued.
DISTURBING CONTENT WARNING. A MAN DIES IN THIS VIDEO
The video below shows a scumbag who got shot for trying to steal. It looks like the guy who blasted him got a good lung shot and hit some blood vessels. Notice the frothy, bright consistency of the blood and how quickly the guy deteriorates once he starts coughing it up. Most likely he aspirated his blood into both of his lungs and ultimately drowned in his own fluids. Not pretty. Fixing this guy would require lots of suction, positive pressure ventilations, endo tracheal intubation, lots of diesel fuel or helicopter fuel to get him to the trauma OR ASAP to get the vessels spewing into his lungs closed. Lesson? Armed robber is a poor career choice.
http://www.liveleak.com/ll_embed?f=02b855f52d8b
Abdomen
Inspect and palpate the abdomen. If your patient reports pain anywhere in the abdomen, palpate that area LAST. You are feeling for rigidity and abdominal guarding, where the patient flexes the abdominal muscles when your palpating causes pain over an inflamed or injured organ. Also look for rebound tenderness, which is pain AFTER you take your hands off the abdomen and the abdominal wall returns to its normal position. This could be a sign of something – like blood – irritating the peritoneum, which is the lining of the abdominal cavity. Look for signs of ecchymosis on the skin of the abdomen. It can indicate severe blunt force trauma to the abdomen or bleeding somewhere else that is pooling in the abdomen.

Flank ecchymosis from blunt force trauma to the abdomen.
Source: http://www.wikidoc.org/index.php/File:Blunt_abdominal_trauma.jpg
If you see something pulsating in the patient’s abdomen, DON’T PALPATE IT. It could very well be an abdominal aortic aneurysm, which means their descending aorta may burst open at any minute. Find out what this patient wants to say as last words to anyone he cares about, because this finding in the field is very grim. Very carefully load him into a stretcher and take a nice gingerly trip to a vascular surgeon to try and fix it.
Trauma to the patient’s upper right abdomen should make you highly suspicious for a liver laceration or injury. The liver is very vascular and can bleed profusely. Keep a keen eye out for shock in these patients. The same thing holds true for the upper left side of the abdomen with the spleen. Watch for distension in the abdomen and signs of shock, indicating an internal bleed.
If the patient has an evisceration, which is where the intestines herniate through the abdominal wall and the skin, soak a dressing in sterile water or saline and place it over the intestine. Cover that with plastic and tape it down. You want to keep the tissue moist. DON’T shove the intestine back in the hole. It’s already been exposed to germs and dirt on the outside and you can make any rupture of the small bowel worse by spilling gastric contents into the abdomen, thus making a bad situation worse. This is not necessarily a life threatening condition, and you may be able to skip over it to continue your assessment. Let the patient’s condition guide you on this.

Evisceration from a knife wound to the abdomen.
Source: http://www.trauma.org/index.php/main/images/C13/
If your patient has been shot in the abdomen, any and all of the above injuries can occur simultaneously. Count the holes, note their positions, and place absorbent dressings over everything to help with bleeding. If you can roll the patient on his side to look for wounds on his back and treat them, do it. DON’T pour hemostatic agents into the wounds. If an evisceration is present, follow the above treatment. Allow your patient to bend his knees when laying supine when he has an abdominal injury. This alleviates some of the pull on the abdominal muscles and wall and alleviates some pain.
The abdomen is a magical, mysterious place where a lot of stuff can go wrong. You have to suspect a lot of different injuries in any kind of trauma because you have different kinds of organs and organ systems all in one compact area. Repeated patient assessments are key with abdominal wounds.
Pelvis
Assess the pelvis by LIGHTLY pressing down on the hip bones (illiac crests) as well as inward. Did I say lightly? If your patient screams at you and tries to choke you out, then there’s probably something wrong. If you feel crepitus with either press, something is VERY wrong and your patient has a fractured pelvis. This is a critical injury because a pelvic fracture can bleed 2000ml of blood in short order. That’s an instant Stage IV hemorrhage with decompensated to irreversible shock as a perverse reward. You’ll need to create a pelvic binder to help stabilize it, reduce bleeding, and reduce the volume of the pelvic cavity for blood to pool. Wrap a sheet, KED, a cut up foam sleeping mat with belt, whatever, under your patient and around his pelvis and secure it so the pelvis cannot be moved around. Very carefully get your patient onto a long board or stretcher and pack voids to minimize movement. Be on high alert for shock and treat aggressively. If there are bullet holes in your patient’s pelvis, the treatment is the same with the additions of counting the wounds, noting their locations, and applying dressings. The video below shows good technique in creating a pelvic binder.
Legs
Inspect and palpate your patient’s legs. In the upper legs, we are very concerned about the femoral artery and the femur. Femur fractures can lose 1500ml of blood pretty quickly, so be prepared to aggressively treat for shock if you see deformity and massive bruising. If a femur fracture is found or suspected, treat it when found, as it is a life threat because of the amount of blood that can be lost.
Pic below shows some good bruising:
A closed femur fracture, which means the bone has not penetrated through the skin and is visible, can be treated in the field with a traction splint. These are not things you carry in your daily kit, so the best thing you can do in the field is to supply manual traction. A patient with a broken femur is likely to present with the injured leg shorter than the uninjured leg. The x-ray below illustrates how the now two-piece femur is out of alignment.

Have one of your team members apply traction by grabbing the foot of the injured leg and pulling downward (caudally) to get the bones realigned. This also helps reduce the pain. Have the rest of the team poke around and find materials to make a hasty traction splint, because it’s going to be hard to have someone holding traction on a casualty you need to drag out of the woods. Below is a great example of the hasty traction splint. Be creative, have fun with it.
Key to any extremity injury is to check for pulses in the extremity south of, or distal, the injury site. On this femur fracture, you can check for a popliteal pulse on the back of the knee, or for a posterior tibial pulse just behind the interior ankle bone (aka the medial malleolus). Do this before applying traction, after applying traction, and after applying the splint. Continue to check for those pulses routinely, especially when you are moving your patient across country. Here’s where to find the posterior tibial pulse and the dorsalis pedal pulse as a bonus.
You want to try and keep the tissue distal the injury perfused as much as you can to avoid compartment syndrome from developing. The leg is a big hunk of meat, and if all of the tissue south of the injury gets starved of oxygen and dies, you are going to have a mess of acids, toxins, and the wrong kinds of electrolytes flood back into the bloodstream when circulation is restored. This can cause cardiac arrest.
If you have an open femur fracture, where the bone is sticking out through the skin, life just got more complicated.

Now THAT is sexy. Doesn’t that look like fun?
Source: http://www.jacknaimsnotes.com/2013/07/image-of-day-19-open-fracture-of-right.html
In the field, it is highly unwise to put traction on this injury, because you risk causing more damage to the vasculature and nerves in the leg by letting the sharp bones slice their way back through the meat in the leg. Furthermore, you increase the risk of infection. So the thing to do here is to tell your patient “Sucks to be you, brah,” then stop any active, life-threatening bleeding (if you did your blood sweep at the start, you’d have found this already, but we’ll do this anyhow) by applying your tourniquet high and tight on the leg. First – but fast – check for popliteal and pedal pulses distal the injury to see if there is any circulation. This helps you gauge how bad the injury is. If no pulses distal the injury, then we know the tissue has not been getting perfused for a while. Apply your CAT-T until the bleeding stops and you can confirm lack of pulse distal of the injury if it was there before. Here’s a video on application of the CAT-T. Strap your Oakleys and Multicam on and enjoy.
Make sure you mark the time you applied the CAT-T. You can do it on the tourniquet, the extremity, or the patient’s forehead. Example: “T 1345” means tourniquet applied at 1345 hours.
Next cover the bone ends with dressing soaked in sterile water, then dress the wound and bandage it up. Get the patient loaded up and pack towels, clothing, whatever you can around the leg to immobilize it. A splint may be in order, but again, NO TRACTION. Just try to keep the thing immobilized.
Any amputation occurring at the upper leg will be treated the same way as the open femur fracture. Stop life threatening bleeding with a tourniquet or tourniquets and treat the patient for shock.
Clinical note: Tourniquets CAT-T versus SOFTT-W? These are both solid items. I like the metal windlass of the SOFTT-W better but find the CAT-T is easier to self apply with one hand, so I carry the CAT-T. Just practice with whatever you decide to carry, and if you are in a group, everyone should be carrying the same thing. Always buy from a reputable source. There are fakes on places like eBay, so be vigilant.
If your patient is laying on the ground with one leg shorter than the other with his toes pointing inward (medially) while screaming in pain so loud that you have just alerted the forces of darkness in a 50 mile radius to your location, you may have a dislocated hip on your hands. Quickly expose the leg and look for any injury. If none is found, then you are narrowing it down fast. Check pedal pulses. Check the pelvis for crepitus and palpate the hip area for crepitus as well. If none is felt, you may be OK for treating for a dislocated hip.

Dislocated hip.
Source: http://emedicalppt.blogspot.com/2011/07/hip-dislocations.html
While painful, if pedal pulses are present and there is no sign of any injury, this is not a life threatening injury. However, the amount of screaming you will hear from your patient will make you want to fix it to shut him up. Grab an extra cartridge from your kit and give it to your buddy to bite on. He’s going to need it. Here’s the Captain Morgan hip reduction technique.
Now, we’re not supposed to do this as pre-hospital providers, and I sure as hell don’t do this in the course of my job. However, if all that’s left of my hometown is a mushroom cloud and the screaming of my tribe brother is calling the drones of the Geheime StaatsPolizei to come over and Hellfire us out of existence, I’m not worried about getting my patch pulled anymore. In other words, only do this in extreme emergencies where there is no other help available. Otherwise, get the patient to the ER / CCP/ base and let the doc or the PA do the reduction.
Once you do the reduction recheck the pelvis, hip area, and pulses. Assess for any swelling or bruising. Make sure you didn’t break anything by fixing it.
If your patient is lying on his back with one leg potentially shorter than the other and the toes on the injured leg point outward (laterally), suspect a hip fracture. This one is very serious because a hip fracture means a femur fracture, a pelvic fracture, or even both.

Hip fracture. Note the shorter leg and lateral rotation.
Source: http://www.utahmountainbiking.com/firstaid/fxhip.htm
You want to immobilize the injured leg and avoid doing anything to it that would open up the fracture even more. Check for distal pulses. Treat with a pelvic binder, packing the voids around the leg, and shock measures.
Further down the leg, you have the tibia (shin bone) and fibula. If these are fractured, you don’t put them in a traction splint like the femur. In the context of a rapid trauma assessment, these may be ugly, but not life threatening. The key is how much the break is bleeding. If it looks like an artery has been damaged because blood is spurting out of it or the calf has swollen into a purple basketball in a closed fracture, you’ll need to fix it right away. If there is minimal bleeding and the patient has other things going on, note the wound and come back to it after you have taken further stabilization measures.

An open tibia / fibula fracture.
Source:http://commons.wikimedia.org/wiki/File:Tibia_%28Shinbone%29_Shaft_Fracture.JPG
In the case of a life-threatening bleed, apply a tourniquet above the knee and tighten it until the bleeding stops and there are no distal pulses. Mark the time, treat for shock, and Charlie Mike.
In a closed tib/fib fracture with obvious deformity, check the distal pulses (noticing a theme here?). If there are none you can try a reduction in the field to get them back – ONCE. Hold the patient’s foot and apply traction by pulling it caudally until it is inline with the upper part of the tib/fib. Check for distal pulses. If you got it right, they’re back. If you missed it, you’re done anyway. Splint the lower leg. Check for pulses after splinting.
Here’s a great example of an improvised splint for the lower leg. Lots of camping gear up on this one. Always be thinking about how you can repurpose your gear for medical use.

Source: http://www.idratherbehiking.com/
An open tib/fib fracture should be treated the same way the open femur fracture was. DON’T perform a reduction. Leave it as is. Check for distal pulses. Stop life threatening bleeds with a tourniquet placed above the knee. Recheck pulses to ensure there are none. Cover the open bone ends with dressings soaked with sterile water or saline. Dress the wound and splint it.
For gunshot wounds and puncture wounds in the legs, if you can control major hemorrhaging with direct pressure, packing the wound with hemostatic gauze and/or hemostatic agents, that is preferable to a tourniquet because you are not cutting off circulation to the entire extremity as you do with a tourniquet. If a tourniquet is your only option or there is just too much bleeding going on, apply the tourniquet above (proximal) the wound site. As before, check distal pulses before and after applying the tourniquet and mark the time it was placed. Dress the wounds with gauze and hemostatic agents. Assess the extremity for motor and sensory by having the patient wiggle his toes. Run a marker or handle of your EMT shears along the bottom of the foot to test for sensory. Note if there are any deficits, as the bullet may have caused some nerve damage.
Arms
Checking the arms is very much the same as the legs. You are looking for life threats and need to stop those as they are found. That’s pretty much damage to the axillary, brachial, radial, and ulnar arteries causing a life-threatening bleed. Check for pulses distal to any injuries as well as sensory and motor function. Attempt to control bleeding with direct pressure, wound packing, and hemostatic agents. If that fails, place a tourniquet proximal the injury and tighten until bleed stops and there are no more distal pulses. Mark the time you placed the tourniquet, dress and bandage the wounds.
Open fractures need to be left as-is. Check distal pulses and motor function of the hands. Stop any life-threatening bleed with a tourniquet proximal the wound. Cover the open bone ends with dressings soaked in sterile water and saline, dress the wound, splint it.
After splinting the wound, apply a sling and a swathe to immobilize the arm. If you are dealing with a clavicle fracture from earlier, now might be the time to deal with it. Best treatment for it is a sling and swathe. No splint needed for the clavicle alone.
If the fracture is located in the upper arm, the treatments are the same for open and closed fractures with the major difference in the splinting. You may need to create a long-board splint and then swathe it to your patient’s body. Below is a nice illustration of a long-arm splint.
Back
Once you have assessed the patient and stopped all life threats while he is supine, maintaining cervical spine (c-spine) stabilization (if indicated), you will log roll the patient onto his side and assess his back. The person at the head of the patient maintaining c-spine directs the call on when to roll the patient. While the patient is on his side, expose his back and look for any deformities or injuries. Treat life threats and note the locations of the injuries. Below is an OK video of a log roll and immobilization of a patient to a long board. The assessment of the back is pretty shitty. DON’T be that nonchalant about it. EXPOSE the back and put your hands on the patient to feel for crepitus or vertebrae that are out of alignment.
Wrapping it up
That pretty much sums up the rapid trauma assessment and the also-rapid follow on assessment. Like before, once all of this is done, treat the patient for shock by supplying O2 if you have it, starting fluid resuscitation, and wrapping him up in blankets. You’ll need to reassess your patient every five to fifteen minutes depending on his status.
While this is a lot of information, practicing assessments can help you get this entire process down in under ten minutes. The goal on any trauma scene is to get the patient stabilized and in transit in under 10 minutes, with the ultimate goal of getting him on the operating table in under 60 minutes from the time of injury. In a grid-down scenario, there may be no place to go for a while, but finding and fixing fast is still something you need to do with trauma. The more blood you keep in the vessels, and the more respiration can happen, the better the outcome for the patient. We’re still focused on stabilizing the patient to get him to some form of definitive care. In later posts, we’ll go over sustained wound care, orthopedics, and other things that will have to be done in the field or in more primitive conditions if there are no hospitals to go to.
TCCC note: This assessment is NOT the TCCC assessment. What we covered would maybe happen in the Tactical Field Care phase and most likely happen in the CASEVAC phase, when more definitive treatment can be done. We’re going to have more on TCCC from some of our contributors that have done it for a living, so stay tuned.
Next up will be documenting your assessment so you can track your patient’s progress, talk to transportation resources and online medical control, or just transfer care to another clinician.





Good stuff!
The best choice was Lebowski’s spare- About had coffee out the nose when I saw that one. A flail segment was a close second.
The tib-fib pic looks about like mine did.
LikeLike
“Smokey, this is not ‘Nam, this is bowling. There are rules.” 🙂
How’d you smoke your tib/fib?
LikeLike
Between floor and steering column of ’69 GMC van-pretty much crushed,17 breaks between knee and ankle.
Medical care wasn’t the same in 1978-spent 3 months in traction,then 30 years with osteomyelitis.
Found a Dr in 2008 that said he could fix the osteo-started the process in Feb ’09,it was over in Nov of ’11.
LikeLike
I somehow deleted part of my comment-my question was supposed to be what is the treatment for a flail segment- I have a friend who has ribs that do not move evenly due to injuries from injury dirt bike riding,and mine don’t move evenly since lung surgery-is that kind of thing common?
The close second was supposed to be another 5.56 round-I hate touch screens-I end up on different sites by leaving a finger on the screen as well as deleting half of posts.
LikeLike
Great question. The flail segment I am referring to is a new onset / acute presentation. IE the patient just got beaten in the ribs with a baseball bat. It implies that a section of rib or ribs has come separated from the rest of the ribcage, which disrupts the normal negative pressure breathing cycle. Furthermore, shards of bone can puncture the pleura and cause pneumothoracies and all sorts of other nicks, cuts, and punctures in the chest and associated vital parts within it.
If you and your friend have healed and are able to breathe relatively normally with your funky ribcages, I doubt there’s any need to fix them. I do not know how common it is, but there may be some folks along in a while that have experience in ortho / trauma / surgery that can give you a better answer.
LikeLike
Treatment is different than the stabilization, back in the day we would use a weighted bag (lead shot filled vinyl sleeve) about the size of a 1000ml IV bag. It never worked as it should. Think about the mechanics of the flail chest and if one segment is moving while the other is not the efficiency of the affected lung is severely diminished as well as bits and pieces of bone are shearing off and falling into the lung cavity, if you do nothing you WILL have a pneumo/hemo eventually.
*My stabilization* is a soft splint of some sort (pillow, sleeping bag, air mattress etc), secured with something…cravats, webbing, rope, duct tape etc, in several spots; top to bottom; around the torso to keep the segments moving together. Just be sure you don’t tighten the securing straps so tight that the chest cant rise. So perhaps prior to the final tie you ask the Pt to breathe in deep, tie off the strap and move to the next. The pillow which is ideal will keep constant pressure on the fractured segments. IV, O2, Pain meds and thorough secondary assessment because of the mechanism of injury call for helo to trauma facility…I assume surgery to repair the segments is the treatment…I’m back on the road before then and we never really have the time to follow up on Pt’s.
FF/Paramedic 22 years…
LikeLiked by 1 person
http://www.ksl.com/?sid=23089284
A bit late for your injury, but becoming more common in the trauma world.
LikeLike
RE: tib/fib – OUCH.
LikeLiked by 1 person
That is one hell of a post.
Outfreakingstanding.
Will link ASAP today.
LikeLiked by 1 person
Thanks CA. 😉
LikeLike
Pingback: Hogwarts: Rapid Trauma Assessment – Part II | Western Rifle Shooters Association·
This article is a reminder of how bad things can get and how unprepared most people really are, myself included. Thanks for the reminder.
LikeLiked by 1 person
Brian Wagner
Thanks for the response.
In my friend’s case,I was just wondering if the old injury could be mistaken for a new injury if there was an accident etc. where he had other injuries to the chest,since when he breathes,his chest doesn’t expand evenly-it’s weird to see and looks like he could be having trouble breathing,but that’s just how it looks. His Dr’s say he’s getting enough O2,and he doesn’t have any health problems-other than it’s kinda creepy to see him breathe when we’re out fishing and he has no shirt on.
In my case,I would guess that since the surgical scar looks like I was filleted like a fish,the EMT would see that I have prior injury which could explain one side of my chest not expanding quite as much as the other. In my case it’s scar tissue from lung surgery that causes difference.
LikeLike
Great post. Mike you rock.
A few shortcuts and things I do.
In a flail chest all of the above duct tape methods are good initial treatment.
Be prepared to manage tension pneumothorax As above.
Respiratory fatigue will be an issue Over time.
Using a BVM to provide assisted positive pressure ventilation will not only help reduce fatigue but can splint the flail segment from the inside. This level of intervention does not require sedation.
If you need to intubate/sedate, you can use an inline cpap valve to maintain internal positive pressure on the flail segment.
For prolonged exfil add in a “nose” in the circuit to add humidity to the air.
Skull- 2nd assessment. I teach to reach up press and wiggle your scalp on your skull. Feel the smooth skull. Just as you can feel a paper edge through another peice of paper, likewise you can feel a the step of a skull fracture, Or the gap of a fracture.
Tension- second assessment. First sign is anxiety followed by SOB. If you have a scope and an awake patient have him say the letter “a” this sound will transmit much quieter on the side with the airspace of the pnumo. It becomes obvious where just breath sounds are harder to hear. If the sound changes to an “ee” (egophony) there is something dense under your scope like blood.
Needle decompression- the needle decompressed tension. Be prepared to decompress more than once if the needle clogs. It a temp solution before a chest tube.
Flutter valves are not needed glove tips not only don’t seal but air will move through the biggest hole. The 14 GA cath is too small to create any kind of sucking chest wound To worry about.
Sucking chest wound. Just put a big sticky monster dressing of choice on it. A sticky mouse trap (unused) works great as well. Gorilla tape, the patients hand on plastic, etc… we teach seal all sides. If they develop tension,
Poke a needle hole in the center of the dressing Or leave a iv cath in the dressing. Standard needle decompression if needed.
If you don’t have the needle and can’t do a standard needle decompression cut as you would for a chest tube. Just tunneling a hole will prevent tension From developing.
An ET tube with a heimlich valve makes a good chest tube substitute. I can write more on light and fast improvised airway kits.
Eviscerated- a post in itself. I use a plastic bag taped on all sides to cover things initially. Remember to insulate in extreme temp environments.
Arm splint- take the bottom hem of a t shirt. Pull it up over the arm in typical splint position. Pin it or tie it to the opposite shoulder. Takes 30 sec to make this splint immobilizer for any clavicle arm or hand fracture.
LikeLiked by 1 person
Great tip on the reduced transmission of vocal sounds in pneumothorax, and the egophany. I’ve never done either, but will try it the next time I find a patient with either who lacks an ETT.
I’ve certainly cut the hole for a chest tube when nursing couldn’t get me the tube in time. Nowadays we just drop in the pigtail catheters instead of the big boy chest tubes–only exception to that is the hemothorax.
I had to decompress an pneumo-abdomen once. The patient coded after a GI procedure to ablate (that is, burn) various lesions in the stomach. After intubation, the RT was over-excited and pushed a little too hard. We could see the stomach swelling but somehow managed to get a pulse back. Follow up KUB had an impressive amount of air in the abdomen, and we could not ventilate the patient. Turned out the patient had a perf in the stomach, and the over-ventilation caused an abdominal compartment syndrome as the perforation acted as a one-way valve. So I dropped an 18g IV catheter in the abdominal wall and we spent around 5 minutes listening to the whistle of air coming out. Darnedest thing I’ve done in a while.
LikeLike
As Keanu Reeves would say, “Whoa….”
LikeLike
um wow….only seen that in a sheep.
LikeLike
Eventually we should get around to a full post on femur fracture management, heres the rough outline for the above pre hospital management that I prefer: Roll or beam lift the patient supine onto a litter, (see indication below) next while applying gentle traction flex the hip and knee to roughly 90 deg and while stradling the patient grip just below the knee apply traction lifting up on the femur. (they wont like it at first) The lower leg is horizontal between your legs, patients foot on your back side so you can just lean back to create traction with your elbows on your knees and fingers laced under the proximal calf, place large firm objects under the knee until you can slip a hand under the pelvis on the affected side because they are hanging from the flexed knee. tape and strap in place. You now have created a traction splint using the patients body weight.
The indication to do traction is in the limb with significant neuro or vascular comprimise. Most patients with femur fractures will find non traction supine on a litter with lots of loose padding and strapping to be adequate immobilization for transport.
Definative low tech care involves 6-8 weeks bed rest with a pin in the distal femur or proximal tibia and traction.
I am not a big fan of the stick in the groin traction splint. The kendrick traction splint is a nice light weight unit but I dont carry it often due to wt and space.
LikeLike
Really old guys will remember Stryker limb splints, which were padded aluminum “boards” with wrist or ankle collars with cords that dropped into slots in tabs at the distal ends of the splint.
These were great immobilization tools and great comfort creators.
Shorter ones for arms, longer ones for legs.
LikeLike
Pingback: Rapid trauma quiz – how we scored | Hogwarts School of Grid-Down Medicine and Wizardry·
Had the opportunity to put this to test yesterday.
A couple blocks from my house I rolled up on an SUV wrapped around a tree in the median. Smoking heavily, driver was already out and lying on the ground.
Single vehicle, MVA SUV vs TREE. Within a minute or 2 vehicle was completely involved.
EMT student (passing driver) had pulled driver from vehicle, 20yo hispanic female, very fit, bloody mouth and chin, aware and responding to questions, so A and C covered. Quick scan for B shows MASSIVE distortion to upper right leg (pretty much the picture here without the bone actually sticking out), torn yoga pants, minimal visible bleeding. Patient complaining of pain in leg. 911 called and no one else in vehicle.
Assess scene safety, patient out of vehicle, talking and breathing, vehicle in flames, rapidly getting worse. EMT student wants to move patient farther away, worried about explosion. I say “wait, I’ll get a board” intending to try to stabilize leg or c-spine, 20 seconds later, he’s already moved her another 15 ft away. So much for that.
Reassess A,C, still tracking, still talking.
Glove up, cut away right pant leg, open fracture, lots of distortion and swelling but no visible bleeding. Quick scan of upper body, back and head, no bleeding. Big red mark, right side of abdomen, minor bleeding in belly button around metal piercing, bloody mouth and chin appears to be related to metal piercings, no active bleeding.
So ABC covered, emts on the way so no attempt to do anything further than visual and continue assessing mental state, breathing, and watch abdomen. Got patient name, age, dob, no existing medical conditions.
Fire arrives and begins extinguishing SUV, EMT arrives and takes over care. C collar, backboard and transport. Crash to transport <25 minutes.
SO…. I've had the CERT medical modules and some home study. The EMT student was a firefighting student with very minimal class time. What I'm kicking myself for:
Scene assessment, I should have verified that vehicle was empty. There was still time when I arrived to rescue someone if they were inside, particularly a child in the back seat. IF that was going to happen it needed to be in the first 30 seconds, after that it was too late. No fire extinguisher in MY truck.
I didn't see the EMT student remove her so can't assess technique, and it WAS the right choice given the fire, but it couldn't have been fun for her, her leg, or any c spine issues.
Further, I don't have a lot of experience with car fires, but I believed we were far enough away, and that vehicles don't usually explode. If we weren't feeling heat, I don't think we needed to move her again especially without good technique. Feedback on this would be great.
Moving the patient the second time. I wish I'd stayed to HELP the guy do whatever he did to move her, or that he'd waited for help. I was only gone to my truck for 20 seconds, but that was enough for him to act. I can't believe he dragged her with that leg… [should have assess PMS on right foot before and after movement]
Not taking control of the scene. After he moved her, I realized that the EMT shirt he was wearing was for a local school, and that he was young, excited, and inexperienced. Help was on the way. We're a major city, less than a mile from the local fire station. 1.5 miles from a hospital.
ABC ok, she's not dying in the next 5 minutes. I should have introduced myself and him and asked for permission to treat. I should have done a quick hands on head to toe. I should have done more to immobilize head. I should have assessed PMS in foot. I feel like I should have said something to him like, "ok, we have time, lets go thru this by the numbers…." but I didn't realize just how green he was and I deferred to him. I'm pretty sure looking back that I have more training, and was calmer than him.
What I feel ok about:
The visual and verbal scan covered the ABCs and I was thinking 'first do no harm'. No need to wing it with help on the way.
My homemade bag will need some reorganization. And I need to do some more familiarization. I had to look in 3 pockets to find my gloves. PACK EXTRA GLOVES. I was supplying him as well. I had a pen for history, but NO PAPER. That didn't F me in this case, with help on the way, but it is an oversight.
What I feel less than ok about:
I didn't have a fire extinguisher in this truck. I've got one in my pickup (2 actually) but nothing in the Expedition. I have a good one now.
No leather gloves. In my pickup I've got leather gloves ready to go in the door pocket, none in this truck. Attempting a rescue would have been unnecessarily dangerous barehanded.
Some other random observations:
I had just added a wristwatch to my car bag. I don't wear a watch anymore and I realized I would want one if I did have a medical emergency. It was REALLY handy to have it strapped into my bag.
Body piercings will cause injury if you are in a high force impact. She had tongue, belly button, and possibly more, and they all ripped skin.
I missed damage to her right arm, and heavy scratches on her chest, that the (real) EMT caught, because HE LOOKED.
Her phone was in the vehicle. If you are counting on using your phone or having someone look at it for an ICE contact, well……. In this case, she was on her way to class and a friend was in the car behind her. The friend could answer questions and called family. Ditto for wallet in a purse.
You really can't have too many gloves in your bag.
They transported her to our level one trauma hospital so I'm guessing the leg was even worse than it looked. That's a 20 minute transit vs 7 minutes to our local hospital.
I need more training.
Anyone who cares to comment, please offer some AAR critique or kudos. I was in the right place with (some) of the right gear, and (some) of the right knowledge. If it happens again, I want to be better prepared in both cases.
thanks,
nick
LikeLike
Nick,
Ya done good. You guys helped the patient get away from a burning truck, you were able to determine her mental status, and found major injury pretty fast.
You proved out that the term “first responder” really belongs to the people who come upon a scene first and call 911.
You guys made a good decision to get the patient away from the vehicle. Your safety comes first, then the patient, then everyone else. By getting her (and yourselves) out of there, you prevented yourselves from becoming casualties as well. Your thinking was on point in at least trying to get her on a board to keep her stable, but you got overruled by youthful exuberance.
The key is to do the best with what you have.
Reminder that the ABCDE assessment mnemonic breaks down like so.
A- Airway – patent?
B- Breathing – adequate?
C- Circulation – radial and/or carotid pulses present?
D- Disability – Mental status – Alert? Responsive to Verbal commands? Responsive to Pain? Unresponsive? (AVPU).
E- Exposure – Physical status – Cut the patient’s clothes and find immediate life threats presenting as deformities, contusions, abrasions, punctures / penetrations, burns, tenderness, lacerations, swelling.
You were successful in determining her mental status and found a pretty major injury in the open femur fracture that is definitely a life threat.
Seeing the other injuries you found on her, what organ systems do you think might be affected / injured? How would they affect your assessment of her?
Good AAR on yourself. All I can advise on skills and gear is that repetition is the mastery of skill. Practice wherever, however, and with whoever you can. Check into your local community college and see if they have First Responder and / or EMT-B training. It’s great stuff.
My hat’s off to you for taking CERT training and also having the courage and humanity to stop and help out a stranger – check that – a fellow American in need.
Bravo Zulu Nick.
LikeLike
Thanks Mike, I’m guessing that NOT second-guessing yourself is a major part of the process, once you have reviewed for lessons learned. Coulda Woulda Shoulda seems like an occupational hazard 🙂
So many mnemonics ! CERT simplifies- so A,B,C is Airway Bleeding, Consciousness. And PMS is perfusion, movement, sensation (IF I’m remembering correctly) and is mostly important for splinting…
START is in there someplace too.
“Seeing the other injuries you found on her, what organ systems do you think might be affected / injured? How would they affect your assessment of her?”
With the large red patch on her right side, I was worried about internal bleeding as a result of trauma to liver (Or other organs). I was watching her stomach for signs of distention, looking for the blood pooling in the skin, and watching for shock.
The bloody mouth had me concerned that she hit the airbag hard, but it seemed pretty superficial, and easily explained by the piercings. No other marks on her face or forehead. I never checked her ears or pupil response, but was definitely worried about brain injury. Best I could do was continue watching her speech and responses.
Of course with MVA I’d suspect whiplash injuries, but with help on the way, I didn’t think too hard about stabilizing the neck, esp after she’d been removed from the vehicle and moved again. She only ever complained of pain in her leg. We did have her lying still.
I missed the right arm but should have looked considering that she had so much damage on her right side. Mainly though, the other guy was on her right and I was on her left. Perfect argument for one person doing a complete assessment (and not assuming competence).
Given the other right side injuries, I should have checked for cracked or broken ribs, but her breathing was good (easy, natural, slightly fast) and I don’t think you could do that with a broken rib. Something for the ER to check though.
With her breathing and responding, and no visible bleeding I could do anything about, I felt her condition was pretty good (other than the massively broken leg.) I was worried about brain injury, and internal bleeding mostly, and couldn’t do much but monitor for changes (and watch for shock).
If I wasn’t sure EMS was enroute, or if I was gonna be on my own for a while, I think my next steps would be cover and immobilize leg and then neck, and a much more thorough head to toe, treat for shock, start tracking actual pulses and respirations, maybe history, at least for current issues, allergies, meds, etc. Basically prep for higher care, improvise backboard, c spine, and splint, try to save some time for when help arrives.
Of course grid down, I’d be prepping her to evac by whatever means, to a safe or triage area and if there were none, then oh boy, we got some reading to do…
thanks for the response, and for the site!
nick
BTW, after Aesop made his post about the single best thing you could do to get ready was to take the EMT-B classes, I checked in my area. There were several corporate programs and a couple of community college based programs. All were about $1200 which actually seems reasonable. My problem was committing to the full day classes several times a week, and then the required clinical time on weekends. I’m looking for something a little more flexible, and there was a program with mostly online classroom with the clinical component live of course. I can’t help wonder if the online is enough, or if the classroom interaction is where the real learning takes place. Any thoughts? (other than something is better than nothing.)
LikeLike
Confidence comes with practice and experience. I think your head is in a great place and you are thinking the right things. Do all the second-guessing AFTER the call. I always knew I had a good partner when he or she would be willing to go over a call play by play after it was over and critique ourselves. Good on you for doing the same.
As for the training, there are online places. Only trust the ones that require you to do clinical and skills in the real world as a requirement for a cert. Anyone that says you can get a cert online-only is not being truthful.
You will miss out by not meeting with a class full of people weekly, because there are points where you break away from lecture and do scenarios and skills. They are a lot of fun because they are the points (outside of real calls) where everything you are learning comes together. Above all, medical care is a human endeavor, and the more people-time you can get, the better.
Like you said, something is always better than nothing, and if online is what you have bandwidth for, by all means, get everything out of it that you can.
Good luck and thanks for being here!
LikeLike
You will not put a significant car fire out with a fire extinguisher. It’s only utility is to put out a fire on an individual or get you to be able to rescue.
Battery and fuel are both explosion hazards.
Finding injury is good but more important is how she is tolerating the injuries. Stable or unstable systems. Air goes in and out. Blood goes round and round. Just make sure that is optimized and everything else is just style points.
LikeLike
@ pa4ortho, “everything else is just style points” is awesome. Thanks!
I can’t help thinking about what would have happened if there had been a baby in the backseat of the SUV. Enough time to get that out would be all I’m looking for with an extinguisher. As it happened, her baby was safe at home.
It’s also clear to me (from the difference in ABC CERT style vs ABCDE EMS style) that so far my formal training is DISASTER based. It’s gonna be a big change (and upgrade) for me to learn the EMS way. I knew that intellectually, but something like this drives it home.
Thanks for the response, and for your other contributions here.
nick
LikeLike
Pingback: Rapid trauma assessment – Part III: You need some SOAP | Hogwarts School of Grid-Down Medicine and Wizardry·
Pingback: Hogwarts: Rapid Trauma Assessment – Part III | Western Rifle Shooters Association·