As of this writing, if you are living in the eastern half of these United States, chances are you are smack in the middle of the Siberian Express cold spell that has temperatures 20, 30, and even 40 degrees cooler than normal.
The winter wonderland it has brought us is bracing, refreshing, and deadly if you are not careful. Let’s take a quick look at hypothermia.
Hypothermia is a reduction in core body temperature below 95°F as measured by a rectal thermometer placed six inches into the rectum. The best way to avoid a thermometer six inches into your rectum is to not get hypothermia. The best way to not get hypothermia is to not do dumb stuff. Let’s look at some prevention before we look at fixing injuries.
Be aware of the macro environment. Watch the weather report and see how cold, wet, and windy it is going to get. If you don’t have the ability to listen to the weather report, consider where you are in the country and what can happen during the specific time of year. February in Miami and February in Vermont would require very different packing lists.
Dress for the worst. Weird things can happen to anyone at anytime. It’s always good to be a little bit paranoid and to have enough gear with you to survive a night in the cold without power. If you go to get milk and bread from the store when it’s 12°F in board shorts and flip-flops, you’ll be dead in a few hours if your car slips off an icy road into a ditch and you get knocked out. In an urban area, dress so you can survive at least a few hours in the cold. In rural areas, dress better than that. Have a get-home bag in each vehicle that has at a minimum a mylar thermal blanket. For pure awesomeness, have a USGI poncho liner, a poncho, and hand warmers to put in your gloves and boots. Also keep your inner scavenger alive and look at your surroundings for anything that can be used as improvised clothing. If you have to rip the carpet and upholstery out of your car to make clothes, do it. Cardboard, canvas, newspaper, rags, whatever. Cover is cover.
Layers. Dress in lots of layers. The air trapped between each layer is great insulation, so the more layering, the better. Avoid cotton (like blue jeans) if you can, because it is hydrophilic and will kill you if it gets wet, especially next to your skin. Plan for an immersion in water and having to dry out as fast as possible. Fabrics of choice are silk, wool, polypropylene, nylon and anything else that wicks moisture. Gore-Tex and Gore-Tex-like water resistant fabrics that allow for moist air to escape but not come in are great outer layers and are relatively light weight. Also cover your head and use a neck-gaiter. If it’s really cold, cover your face. Brands like ExOfficio, Mountain Hardwear, and Arc-Teryx make nylon hiking clothes, and like anything else, prices range from affordable to Gucci-level.
Don’t do dumb stuff. This poor woman did some dumb stuff. She was fit, good looking, and let hubris get the best of her, so now she’s dead. She went hiking in the White Mountains of New Hampshire by herself in February. She thought she was bigger than Mother Nature and she got spanked. Worse, she fired off an emergency beacon and put a bunch of other people’s lives at risk to come save her for being dumb. When they found her, she was a human popsicle. Mother Nature ALWAYS has the upper hand. Never forget that.
Eat and drink a lot. Best medical advice I’ve ever heard. Of course, booze is not what should be consumed, but fluids. Eat plenty, including higher fat foods (yes!) if you know you are going to be in the cold for extended periods of time. Your body needs that extra fuel to run its metabolism at a higher rate to keep you warm.
Pack a mix of protein and fat-rich foods for the slow burn and some carbs for the fast burn. Think meats and nuts for the proteins and fats (I also pack some extra virgin olive oil) and things like honey and jam for carbs. The carbs will serve you well in emergencies where you need to get calories into someone fast. The honey and jam are good items for your medical kit to treat hypoglycemia in the field, too.
Dehydration turns your blood to the consistency of ketchup, and that’s not a good thing if you need nice, warm blood circulating through your body to keep vessels open and tissue perfused. Hydration formation people!
Sometimes, you don’t do any dumb stuff and just get stuck in a bad situation. You can get hypothermia when it’s 70°F outside in the right circumstances. It just happens more slowly than at -10°F. You lose heat 24 times faster in water than in air as well. If your clothes are soaking wet, that’s kind of the same thing.
Hopefully these preventive measures minimize your pain, but if things start going wrong, let’s look at how to treat the issues.
Hypothermia
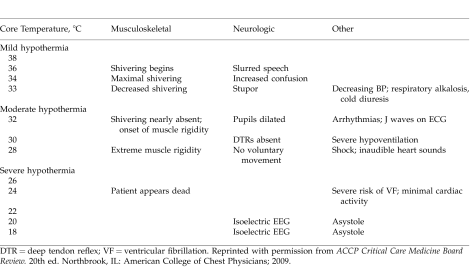
There are multiple levels of hypothermia:
- 90-95°F = mild hypothermia
- 82-90°F = moderate hypothermia
- <82°F = severe hypothermia
- <77°F = cardiac arrest / ventricular fibrillation
Signs and symptoms ([°C x 9/5] + 32 = °F)
A patient with hypothermia stumbles, fumbles, mumbles and grumbles. So if you have someone that has been in the cold for awhile and he starts doing all of the above, stop and check him out. Know the difference between that and what I call “frozen face syndrome” which is what you get after walking the dog on a cold morning and you can’t talk well because your face is half frozen, not because you are getting goofy from a low core body temperature. However, let that be a clue to yourself that it’s pretty cold and you might want to cover your face to avoid cold injury.
*SAFETY NOTE: If your buddy presenting with hypothermia signs and symptoms is armed, you will need to disarm him. He is mentally impaired and could be a danger to himself and others. Keep this in mind.
A key symptom to watch for with a patient in mild hypothermia is shivering. This is the body’s natural response to cold and it is trying to generate heat. If you’ve done nothing for this patient and he is still in the same environment and he stops shivering, this is an ominous sign that he is slipping into moderate hypothermia. People stop shivering when they run out of calories.
If your patient starts trying to take his clothes off while he is whacked-out from hypothermia and not from consciously trying to rewarm, this is known as paradoxical undressing, and things are going south quick. From there, your patient can go into severe hypothermia and risks unconsciousness, cardiac arrhythmias, and possibly cardiac arrest / death.
Treatment
Ideally, get the patient out of the cold environment in all cases of hypothermia. If he is in moderate to severe hypothermia, be very careful in moving the patient around, because you can trigger a lethal cardiac arrhythmia from too much jostling.
If the patient is bradypneic (inadequate breathing), use a bag valve mask or good old fashioned mouth-to-mouth (with a pocket resuscitator) to assist with ventilations.
If your patient has stopped shivering but is conscious and can swallow, give him those fast-absorbing carbs to get calories in him to get him to shiver again. Stimulating him to shiver is warming from the inside, which is more effective than any kind of external warming. Get him doing situps in a sleeping bag if he can’t run or walk. If he can run or walk, get him moving to try and get the metabolism going again. Feed honey. Keep him running. Have him run and find wood. Have him run and stack the wood. Have him set the wood on fire and run around the fire. Feed more honey. Run. Eat. Run. Eat. You get the idea.
If your patient gets immersed or soaked, strip the clothes off and dry them out using air as fast as possible. Follow the procedure in the paragraph above while waving clothes above your head like a helicopter to speed them drying out.
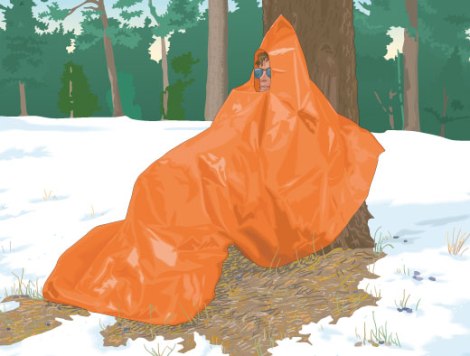
Alternatively when the patient is exhausted drape a poncho over him and have him Indian squat or lean on a tree wearing it. Light a candle or small stove or oil lamp on a rock on his lap. Steam vents off the wet clothes in the sauna. Feed him more honey and jam. Keep the calories coming. Keep an eye on him so he doesn’t set himself on fire.
If the patient is too far gone to eat honey and run, cut off the wet clothes and wrap him in layers (sleeping bags, poncho liners, wool blankets are best) and then get a vapor barrier around all of those layers. A mylar blanket or Gore-Tex is appropriate. This is called passive rewarming. Focus on the torso, head and neck first, because that’s where the important organ systems are and if one of those dies, your patient dies. Life over limb is the key operating principle. Take care when warming the limbs back up to not allow for a flood of acidotic, cold blood to shoot back into the torso. Go slowly and don’t rub them. Wrap them and warm them.
Check radial and carotid pulses. If they are absent, DON’T start compressions yet. Keep warming and ventilating the patient for three minutes. Check the carotid artery for a pulse again. If it is absent, then start CPR. If there is a pulse at the carotid, continue to ventilate and warm. The key principle here is that a patient is not dead until he is warm and dead.
*CLINICAL NOTE: There is an advanced cardiac life support (ACLS) piece to this that I am skipping, because it requires a cardiac monitor / defibrillator and specific actions based on the patient’s core temperature being below and above 86°F. If someone shows up with the equipment, drugs, and a rectal thermometer, they should know what to do here.
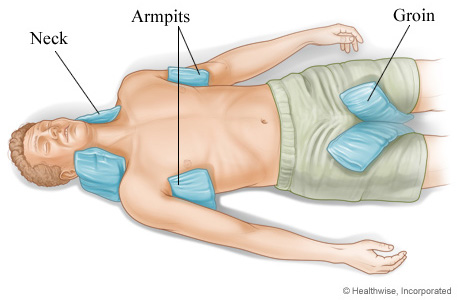
Pack hot packs, canteens or Nalgene bottles full of hot water at the groin on the femoral arteries and in the armpits at the brachial arteries. Make sure to avoid direct skin contact with the hot packs (if they actually work) to avoid burns.
If you have IV supplies and fluids, give a 250-500cc bolus of warmed normal saline or Lactated Ringer’s followed by a saline drip. Passive rewarming with the addition of these two items is called active rewarming and is most appropriate for more serious cases of hypothermia. For warming IV fluids in the field 2 MRE heaters wrapped in cardboard surrounding the IV bag I will be effective. You’ll want to insulate the IV line as well or wrap the line around the patient where body heat can help keep the saline warm. If you have a fire pit with rocks, place the saline bag on the warm rocks, but keep an eye on it. You don’t want to melt the bag. If you have a car or truck, put the defroster on full heat and set the saline bag on the dashboard above the vent. If you have electricity and a microwave, use that.
A great field mod for monitoring your patient’s core temperature is to wrap the probe (not the sharp one, perforated bowels suck) of a wireless digital BBQ thermometer in a nitrile glove and insert it rectally in your patient. Have the medic on the team carry the wireless receiver, which will show the patient’s core temperature steadily, thus negating the need to continually stop, unwrap the patient and check his temperature, thus exposing him to cold air. You will never think of BBQ butt roast the same way ever again.
The best treatment of all is to get the patient evacuated to a warm, dry place where advanced care can be performed, specifically the cardiac component. Again, a patient is not dead until he is warm and dead.
Frostbite
The quick difference between frostbite and non-freezing cold injury is that frostbite happens at temperatures below freezing and results in the actual freezing of the tissue. Cold injury is similar, but the tissue doesn’t freeze, however it is still a serious condition that can wreak havoc on a person. The mechanism for injury in both of these illnesses is the body’s natural response to cold, called shunting, where it constricts peripheral blood vessels in the limbs and digits to keep blood in the torso and head, where the vital organs live. If you couple the vasocontriction with cold temperatures for significant durations, tissue perfusion breaks down and the tissue can become necrotic. Anyone with pre-existing conditions that cause vascular compromise, like high cholesterol or diabetes, is going to be more prone to cold injury. The same thing holds for a trauma patient. He is already shunting because of his traumatic injury, and cold is going to double down on that. Be very aggressive in watching for and treating hypothermia and cold injuries in trauma patients.
Signs and symptoms
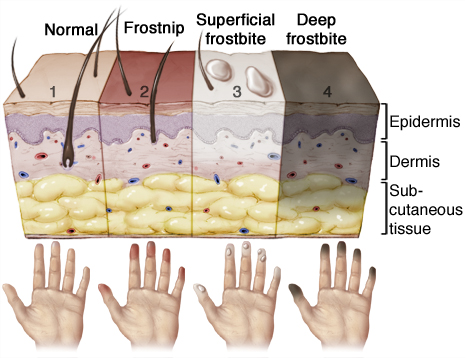
Cool, cold, and painful areas are on their way to frostbite. Numb areas probably have it. Frostbite has a few different looks depending on whether or not the patient is still in the cold or if he is in a warm environment and the frostbitten areas have been thawed. Here’s a quick look at the different phases of frostbite and how they present, from superficial to deep.
Both superficial and deep frostbite will present white and waxy when cold. After thawing, superficial can be white, red, or purple with blisters. Deep frostbite is going to get dark purple or black, because most likely the tissue has been severely damaged if not outright necrotized.
Here are some hands and feet.
Those fingertips look like gangrene has set in and are most likely toast.
These feet are pretty bad, and the tips of the toes look like they are on the margin of gangrene, but this patient may be OK in the long run.
Lots of pain in the affected area as it thaws out is a symptom of frostbite.
Treatment
Like hypothermia, your first course of action is to get the patient out of the cold environment and out of any cold, wet clothes.
If you have them, give pain meds before you start rewarming. NSAIDs, Aspirin, Tylenol, and even morphine sulfate IV if the the frostbite is severe enough in both depth and spread. Aspirin is extra good here because of its anti-platelet properties as well as its analgesic effects.
Rewarming
If there is a possibility that you have to transport the patient after rewarming and the affected areas will refreeze, then DO NOT perform rewarming. Wait until you get to a place where the rewarmed areas will stay warm. If the areas refreeze, it will be a worse outcome for the patient.
For superficial frostbite, start passive rewarming and add hot packs to the axilla, groin, and neck. You want to try and help heat up the blood and get the vessels to dilate, returning blood flow to the affected areas. While the picture below is the placement of icepacks for hyperthermia, the thinking is the same for heatpacks to help alleviate superficial frostbite.
For deep frostbite, the best medicine is immersion in a 104°F whirlpool bath for 30 minutes, then drying and dressing the damaged tissue. Splint as needed. Your patient is going to be in a lot of pain during the bath, that’s why you gave pain meds before.
A key concern with the frozen tissue is possible blood clots (thromboses) after rewarming. A blood clot that ends up in a coronary artery, a pulmonary artery, or a cerebral artery can make for a very, very bad day. Know the signs and symptoms of heart attacks, pulmonary embolisms, and stroke, as well as for a venous thrombosis. Dextran and Heparin are meds to consider if you are properly trained in their administration and know precautions and contraindications for each in this situation.
The longer-term wound care for frostbite is similar to burn care, but there is a significant amount of time – like days to weeks – needed to monitor the damaged tissue before doing any debriding. Don’t debride anything in the field. Wait until you get to definitive care and can get a few more eyes on the patient.
Non-freezing cold injury
This injury is frostbite’s evil cousin, and as stated earlier, it is a cold injury to the tissue that occurs in wet environments at temperatures above freezing. This injury is also known as “Trenchfoot” named after the condition soldiers would find their feet in after days wearing boots in cold water-filled, muddy trenches.
Signs and symptoms
Like frostbite, the initial injury will appear white and waxy while cold, but upon thawing, will present as two possible injuries once warmed.
Chilblains – The injury site is hot, red, swollen, itchy and painful. It can happen in under 12 hours of exposure to the cold and wet conditions, but can also resolve in as little as 24 hours with the proper care.

Source: “Wintertenen” by Sapp – Own work. Licensed under Public Domain via Wikimedia Commons – https://commons.wikimedia.org/wiki/File:Wintertenen.jpg#mediaviewer/File:Wintertenen.jpg
Pernio – These are thin, necrotic plaques on the tops of the hands and feet that appear after more than 12 hours of exposure in cold, wet conditions. They are painful and will slough off over time. And time can mean anywhere from a few weeks to a few years.

Source: http://advocatesforinjuredathletes.blogspot.com/2012/11/environmental-cold-injuries-specific.html
Treatment
Pat the feet dry, elevate them and warm the patient using passive or active rewarming depending on his condition. Administer pain meds and keep the patient off his feet. Supine in bed is best.
Unfortunately the best thing for healing trench foot is time. If the patient is unable to walk, he should be evacuated to definitive care where adequate rest is possible.
The best thing for trench foot is avoidance. Good footwear, copious sock-changing, and airing the dogs out is key. Massaging feet during down time to get blood flow back up helps.
Nifedipine, a calcium channel blocker that helps cause vasodilation, has shown some promise in reducing the duration and severity of chilblains.
In closing
The best way to treat hypothermia, frostbite, and non-freezing cold injury is preparation and avoidance. Spend extra time planning and preparing for some contingencies for freezing wet conditions on every outing. It could save a finger, a toe, a nose, or a life.
– IvyMike and pa4ortho
Homework
Eat well, drink lots of fluids, and check your cold weather gear. Build a get-home bag for your vehicle that has the stuff in it to keep you warm in the worst winter your area can serve you up. Get some quality socks. Buy once, cry once stuff.
Download and read this great presentation from WildernessMed.org on hypothermia and cold injury.
References
1. United States Special Operations Command. (2001). Cold Illnesses and Injuries. Special Operations Forces Medical Handbook. (pp. 6-43 – 6-47). Retrieved from https://www.dropbox.com/s/2b4rgh3irny27t5/SOF_Medical_Handbook.pdf?dl=0
2. North Carolina Office of Emergency Medical Services. (2014). Hypothermia / Frostbite. EMS Patient Care Treatment Protocols for NC EMS Systems. (pp. 130-131). Retrieved from http://www.ncems.org/nccepstandards.html
3. Rustin, M.H. A. Dr. (11 October 1986). Nifedipine in the treatment of chilblains. British Medical Journal. Retrieved from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1341713/pdf/bmjcred00256-0025b.pdf








Reblogged this on Starvin Larry and commented:
Good things to know-avoid having your hands and feet look like the pics-dress for the weather-and always carry extra dry clothing including multiple pairs of socks. I wear wool socks in winter for two reasons- first is they are warm-second is wool is still warm when it gets wet.
LikeLiked by 1 person
Pingback: Hogwarts: Hypothermia And Cold Injuries | Western Rifle Shooters Association·
Nothing on using another persons body heat to rewarm?
I had mild hypothermia as a kid (around age 12) while winter camping when I got wet crossing a creek. I barely made it back to the cabin. My dad stripped me down and got in a sleeping bag with me. He was like a giant hot water bag. Fixed me right up…
LikeLiked by 2 people
Got us. Damned good point. Thanks.
LikeLike
Long, long ago I read in a backpacking article that the mark of a true “trail buddy” is that he will let you put your freezing feet on his bare stomach to help rewarm them.
Avoidance is indeed the best bet…
LikeLike
Thanks for trying to educate us, IvyMikeCafe. I’ve already learned way more than in any FA class I’ve attended. Most of those have been a joke, but I got the certification. In the Red Cross class I did learn CPR and how to sling an arm.
LikeLike
Pingback: Wednesday Weapons Website of the Week: GridDownMed.com | WeaponsMan·
H/T to Weaponsman for bringing me here. A quick perusal tells me I’ll be spending a lttime here both refreshing my knowledge and learning.
Re hypothermia. A navy corpsman attached to 1st Recon in Nam, I got the first stages of hypothermia while on a long patrol during the monsoon season. Temps were in the mid-50’s and it rained day and night. A scheduled 5 day patrol had turned into 7 days because of the weather. We were running out of food. However I always carried and saved a bunch of beef jerky for possible patrol extensions. It paid off. Although I recognized the symptoms, I don’ t believe we got much training for hypothermia. Not supposed to happen in the jungle is it?
LikeLike
Good point, highlights the dangers of cotton in wet moderately cold environments.
Skin is about 84-86 deg F anything colder is all about time and conduction. Calories delay this by fueling shivering and muscle movement.
You can get hypothermia in 75 deg water if you are in it long enough.
Wet cotton is worse than bare skin due to increased conduction and evaporation heat loss.
Mix fats and carbs with honey as a quick emergency boost when neeed. Regular food intake.
Dehydration dramatically alters the ability to regulate heat.
Case Study:
Was training an amature group once where 2 gals wore cotton long johns. It was wet, 10-20 mph windy, and in the 50s. After just 2 hours in that cold they both went down. Uncoordinated, weak and shivering with mild mentation changes. Both were told not to wear cotton. Both were told to eat. They wore cotton because it was soft and pretty. They did not eat or drink as they did not want to go #1 or #2 in the woods. Well they did not get much privacy as we were quite remote. Fed em honey and water, forced them to get up and walk supported for about 1 mile back to “camp” got them stripped down and doing sittups in sleeping bags. Warm drinks with sugar content, MRE carbs followed by fats.
Full recovery after a few hours and resources diverted. Entirely preventable with the right gear and training. Without outside intervention, lethal. Of note the group of about 30 did great all day in the cold except the only 2 with cotton on.
LikeLike
Several have mentioned what has become formally adopted by the military. It is called the “Naked Ranger Buddy”. No it is not part of Clinton’s, Don’t Ask Don’t Tell policy and it does work. If someone presents with hypothermia symptoms and no warming tent is available, strip the victim of clothes, put him in a sleeping bag and then a lucky troop of normothermic temperature strips and gets in with them. Just remember, no spooning is allowed because spooning leads to forking.
LikeLiked by 1 person
😀
LikeLike
good input, works well….. as for me you can keep that thing holstered with shorts on.
LikeLike