Today we’re covering burns, at request from one of our readers (sorry for the delay, fellas). Each year approximately one million people in the United States seek medical care for burns, approximately one-third of these in the emergency department (ED). Although the vast majority of injuries do not require hospitalization, severe burns can lead to significant morbidity and death.[1]
Here are the numbers for survival rates and demography.
Selected Statistics: 2003-2012 Burn Admissions to Burn Centers
Survival Rate: 96.6%
Gender: 69% male, 31% female
Ethnicity: 59% Caucasian, 20% African-American, 14% Hispanic, 7% Other
Admission Cause: 43% fire/flame, 34% scald, 9% contact, 4% electrical, 3% chemical, 7% other
Place of Occurrence: 72% home, 9% occupational, 5% street/highway, 5% Recreational/Sport, 9% Other [2]
All things being equal, if you managed to get to good definitive care, your odds of survival are pretty good – when the grid is up.
There are approximately 123 burn centers in the United States as of 2012.[3] These hospitals are highly specialized in the research, development, and application of severe burn treatments. Many times, the path to definitive care for a severe burn patient starts with basic or advance life support in the field, rapid transport to a Level I trauma hospital for stabilization and more advanced treatment, and critical care transport to a burn center for definitive care. That chain of care depends on some of the best talent and equipment that money can buy. In a grid down scenario, that may be hard to come by and we hope to provide some information that increases a burn patient’s outcome if only more basic care is available.
Preparedness

Looking at the metrics above, when the grid is up, you can see that most burns happen in the home from either flame or scalding. What I have found in the field is that most burn patients need better preventative education about; the hazards of using a charcoal or propane grill as an auxiliary heater in the cold months, the use of gasoline as an accelerant for a bonfire, a Dutch oven on a stove top as a baby bath, and replacing the 9-volt battery in the smoke detector. There is also the “hold my beer and watch this” factor that seems to afflict young white males heavily during prime mating years that can inspire a young man to insert butane in his rectum to make his blue darts more spectacular than his fraternity brothers’. Our future, folks.
Then there are the meth-heads and other assorted Darwin candidates that create HazMat sites everywhere they make their poison, smoke it, take off or nod off, and self-immolate.
From a standpoint of you, dear reader, most of you have figured out to not hang around in stupid places with stupid people doing stupid things, thus, your likelihood for a burn has been mitigated by your ample use of grey matter. Oh, and don’t smoke in bed or with oxygen on, either.
The best way to not get burned is to avoid places where there are lots of volatile and flammable things flying around. If you work on an oil rig, in a petroleum refinery, an ammunition plant, a chemical factory, a nuclear plant, or an engine room, chances are you’ve been immersed in OSHA regs accompanied with hours of brutally dull PowerPoint slides and bad movies reminding you to do the right things to avoid burns while at the same time not sexually harassing or inflicting micro-aggressions on your co-workers. Furthermore, you most likely have people on staff that are at a minimum, trained to provide basic life support and wound care in the field.
The key to avoiding burns is to make sure you assess where you are going and what you are doing. If you will be in an environment where high-pressure, flammable aerosols will be ignited and pointed at something, or on a camping trip with 300 pounds of Tannerite and powdered non-dairy creamer, make sure you pack some burn care gear in your kit and have some training for treating burns. If you are just going fishing down at the river for an afternoon, then you stand a pretty low chance of catching the heated vapors.
If the grid is down, then it’s going to be game on with increased likelihood for burns. People get very creative with ways to heat and light their homes, cook their foods, and heat their water. People rarely practice using their auxiliary power equipment when the grid is up. They do poor jobs at rotating or stabilizing fuels. They Jerry-rig things together that are outright dangerous. You combine these together with the stress of a grid down environment, the possibilities for harm are almost endless.
Anatomy and physiology
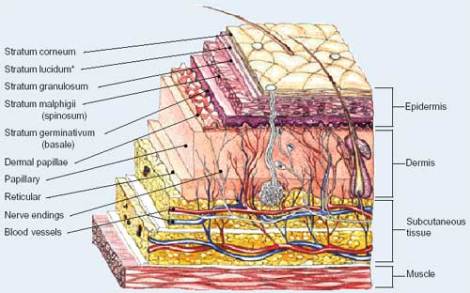
Let’s talk about our very good friend, the skin. It is also known as the integumentary system, or sometimes just the integument. It is a barrier that keeps bacteria and infections at bay, helps us control temperature, prevent fluid loss, and provide sensation to help us get around in the world. It also happens to be the largest organ of the human body.
The skin is composed of three layers:
Epidermis: The thinnest and outermost layer of the skin, it is composed of dead and dying skin cells that are constantly being shed by the body. It lies on top of oil glands in the dermis that secrete sebum to keep the epidermis moist and pliable. If you are not getting enough sebum, your skin gets dry, flaky, and ashy.
Bill Burr explains how it works pretty well. Lotion, people. NSFW…
Dermis: The dermis is below the epidermis and contains blood vessels, oil and sweat glands, and nerve endings. Let’s repeat – NERVE ENDINGS. These are going to play a large role in burns and burn care. The sweat that is secreted by the sweat glands and evaporates on the skin is a key factor in keeping you cool and controlling body temperature. The wet skin acts as a radiator of heat as the body opens up the vessels in the dermis to allow more blood to flow to dump heat while at the same time, picking up a little cooling effect from the wet skin. Flushed, pink skin from your workout is this process at work.
Subcutaneous tissues: This area is composed of adipose tissue – aka fat – and connective tissue. It is a layer of insulation that helps both conserve body heat and radiate body heat depending on shunting or pushing blood behind it or in front of it respectively.
There are underlying structures beneath the skin, which in very basic and general terms, are the muscles (faschia), nerves, tendons, bones, and organs. These are areas that can be affected by very deep burns. Electrical burns can cause all sorts of havoc down here as well.
Burn types
There are four major types of burns. For the sake of brevity, we are going to cover blast wounds in another post, as they are instant multi-system trauma that deserve to be covered in depth.
Speaking of trauma, burns are considered trauma. Therefore, you should apply your rapid trauma assessment in the field and treat life threats accordingly. Do not get hung up on the gore you may see in front of you because your patient may have another, more acute life-threatening injury that you will need to deal with.
Thermal burns
As noted in the stats above, these are the most common forms of burn in the US. These are the burns that you get from contact with something that is a lot hotter than you are. Key to how they happen is the ability of the heated substance to hold heat energy. When you stick your arm in a 350 degree oven to pull the chocolate chip cookies out, it’s definitely hot, but the heated air doesn’t burn your arm immediately because air cannot hold large concentrations of heat energy. If you grab the 350 degree steel cookie sheet with your bare hand, you are going to get burned immediately because the dense steel can store more heat energy than the air / gases. The same thing applies for oils, water, and other liquids. Sticking your hand in a 350 degree deep fryer is going to leave a nasty mark.
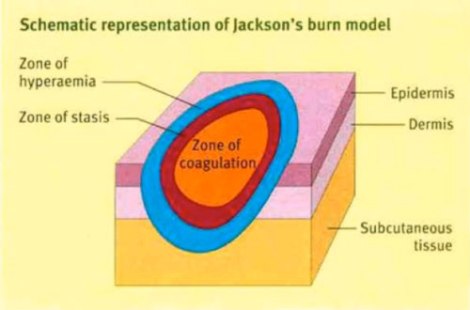
A thermal burn is the rapid transfer of heat energy from the heat source to the tissues of the body. When a substance heats up, the molecules within it move very rapidly, and in tissue, will cause cells, proteins, and membranes to break down and kill the cell, causing coagulation. This process is called denaturing and is very similar to what you see when you cook an egg and watch it transform from liquid to solid.
Once tissue is burned, you have three zones that you are concerned with.
Zone of coagulation: This is the area that experienced the longest and most intense contact with the heat source and the cells within it have denatured, causing coagulation and thromboses in the blood vessels. this area is the most damaged.
Zone of stasis: This is the area just outside of the zone of coagulation and it is marked by inflammation and reduced blood circulation.
Zone of hyperemia: This is the area outside of the zone of stasis and has increased blood flow.
Together, these three zones are the processes that make up the core of Jackson’s theory of thermal wounds, which helps explain the physical effects of high heat on living tissue.
The body has a four-phase response to burns.
The emergent phase – this is what happens immediately after the burn. The body dumps adrenaline (epinephrine), noradrenaline (norepinephrine), and dopamine (collectively, these substances are called “catecholamines“) into the circulatory system and activates the fight-or-flight – aka- sympathetic nervous system response. Heart rate and breathing rate go up, peripheral blood vessels constrict causing hypertension, and patients get anxious. When you think about it, grabbing the hot handle of an iron skillet feels like getting smacked in the hand with a blackjack, and your body doesn’t know if it wants to smack a dude or run away. Either way, your behavior has changed and you are thinking differently at this point.
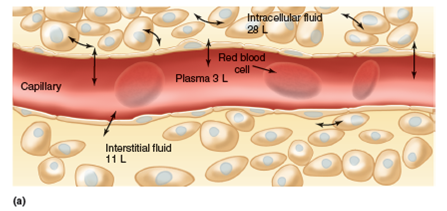
The fluid shift phase – let’s do a little basic anatomy very quickly. The human body stores fluid in two major classifications.
- Intracellular fluid – it sounds like what it is. Fluid inside of the body’s cells. It makes up about 60% of the body’s water content.
- Extracellular fluid – same as above, it’s all the fluid outside of the cells, but it’s broken into three compartments and makes up about 40% of the body’s water content.
- Interstitial space – This is the area within the tissue where the cells float around in interstitial fluid.
- Intravascular space – This is the fluid within the blood vessels, capillaries included.
- Third space – This is the area that doesn’t store any physiologically significant amount of fluid normally, but is an area where fluid can accumulate should there be a derangement in the normal intracellular and extracellular fluid stores.
In the fluid shift phase, in burn cases where more than 20% of a patient’s body surface area has been burned, fluid is going to shift out of the intravascular space and into the extravascular space, near the burn area. This phase lasts approximately 24 hours, and peaks at 6-8 hours after the initial burn.
This fluid shift is cause by the damaged cells releasing agents that trigger the inflammatory response of the body to the burn. Blood flow increases in the capillaries near the burn area, resulting in their increased permeability and proteins, electrolytes, and water being released into the third space.
The hypermetabolic phase – this phase is the point where the human body goes to work and starts trying to repair the damage from the burns. It means that the body will be in overdrive and need lots of nutrients and calories to make what it needs to heal the burns. This can last from days to weeks depending on the severity of the injury.
The resolution phase – this phase is where the scar tissue is created and the patient can start rehabilitation.
Electrical burns
Electrical burns will show up at the entry and exit points of the current, where the skin has a high resistance to electricity. Key factors in severity of electrical burns are the amount of current, voltage, and duration to which the patient has been exposed. If any of the three are high, suspect significant injury.
Electrical burns will travel through the body and cause burn damage to internal organs and tissues. Furthermore, the current can disrupt the normal electrical conduction of the heart and put the patient in a lethal cardiac arrhythmia. If you are treating an electrical burn patient, you are also treating a cardiac patient. Always keep that in mind.
Chemical burns
These burns are not caused by thermal or heat energy transfer, but by chemically denaturing the makeup of cell membranes, thus causing cell death. The chemical has to keep destroying layer after layer of cells in order to get to the deeper layers of the skin and subcutaneous layer.
If you can, try to determine whether a chemical burn is caused by an acid or an alkali, because this can predict the severity of the burn from the beginning.

Coagulation necrosis from an acid burn.
Source: http://www.ijburns.com/article.asp?issn=0971-653X;year=2014;volume=22;issue=1;spage=22;epage=32;aulast=Sarabahi
Acids tend to burn through coagulation necrosis, where as the acid burns the tissue, it forms a coagulated, insoluble layer which tends to limit any further burning.
Alkalis tend to burn using liquefaction necrosis, where the alkali liquifies the tissue, allowing it to penetrate deeply, rapidly.
Below is a pic from an experiment by an ophthalmologist who dipped pig eyes in sodium hydroxide (lye) on the left and 95% sulfuric acid on the right, to illustrate the difference of liquefaction necrosis versus coagulation necrosis. While both are heavily damaged, the eye dipped in lye is pretty much destroyed. Check his site out, he blows up pig eyeballs with firecrackers. My kind of instructor.
Remember, even Tyler Durden used eye protection when with messing with chemicals. Yeah.

Radiation injury
This is what happens when a patient is bombarded with an unnatural concentration of radiation for a period of time. Radiation can disrupt cells and cellular metabolism through the ionization of atoms within the cells. Cell damage is repaired, or the cell dies, or the cell begins to reproduce abnormally (which is cancer). The cells most affected by radiation injury are the ones that reproduce the fastest, like the cells in bone marrow that produce red blood cells, white blood cells, and platelets. It also includes the testes and ovaries, unfortunately.
***
Brass (irradiated) testicles note: The Hogwarts’ faculty highly recommends reading “Nuke the Pilot.” An account of an F-84 driver who was a human guinea pig, along with several other aircrews, the USAF decided should fly their planes through the Mohawk shot during Operation Redwing in 1956. His description of radiation exposure is bone-chilling and that he wrote about it in 2013 tells you he is as hard as woodpecker lips. Bravo Zulu, Major Evans.
***
Key to avoiding radiation injury is awareness of what kind of radiation is possible and where. Key factors driving radiation injury are duration of exposure, distance from exposure, and shielding from exposure. You always want minimal of the first, and maximum of the two latter.
There are three types of radiation, or particles that we are concerned with.
Alpha particles – these are commonly emitted by substances like uranium and the Americium in your smoke detector. Alpha particles from alpha decay are found in radon gas, which is unfortunately found in basements in parts of the country.
Alpha particles can be stopped by paper and even the epidermis but can be dangerous if inhaled or ingested. Fortunately, they only travel a few centimeters, so the further away from an alpha particle source you are, the better off you will be.
Beta particles – these are emitted by byproducts of the nuclear fission reaction in nuclear power plants, like spent fuel rods. Beta particles can be stopped a tin foil, and if not stopped, can penetrate clothing and into the skin, where it will ionize atoms and cause problems. They can travel 6-10 feet, so you can see that enhance shielding and distance are going to be needed to mitigate injury risk. Time to test that tin foil hat, yes?
Gamma particles – aka gamma rays, these have the greatest penetrating power and can go right through an exposed human body, causing problems in every cell they touch. Shielding for these is inches if concrete, several feet of dirt, and inches of lead. These are common at the core of nuclear reactors and from nuclear bombs. Very nasty stuff. Avoid at all costs.
Burn depth
Superficial – otherwise known as a First Degree burn, it occurs in the epidermis, but touches on the living parts of the epidermis, so there is redness, swelling and pain, but heals without issue. A mild sunburn, even though technically a radiation injury from ultraviolet radiation, is a great example.
Partial thickness – otherwise known as a Second Degree burn, this goes deeper into the dermis. With the extra nerve endings in the dermis, these can be quite painful. They will present with redness, swelling, and blisters, but full recover is very likely with proper treatment and care.
Full thickness – otherwise known as a Third Degree burn, this has gone all the way through the epidermis, dermis and into the subcutaneous layer or even into the muscles and bones. Where the skin is that damaged, the burn is not painful because the nerve endings have been destroyed. The part of the skin that can regenerate has been destroyed and massive scarring will occur if skin grafts are not used. These can look black, dry, and leathery, white and dry, charred, and several other ways. One look at one and you know it is serious.
Fourth degree burns is an “unofficial” term for full thickness burns that completely burn through soft tissue and sometimes even bone. These are as bad as they sound. Amputation and death are not uncommon in burns this severe. The photo above is from a man who reportedly picked up a live high-voltage electrical line with his bare hands. Just no.
%BSA
Percent body surface area, (%BSA) is a tool to measure how much of a patient’s body has been burned combined with burn thickness, to help determine the severity of the burn.
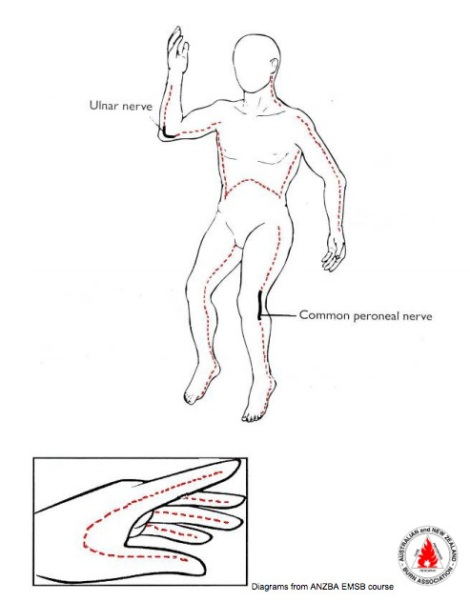
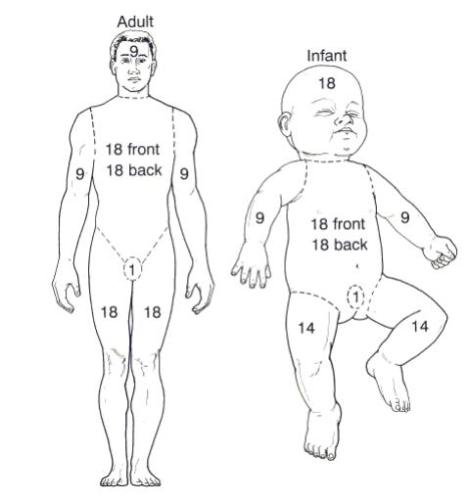
Rule of nines – this system is a relatively handy and fast method to determine the extent of the patient’s burns. It uses a factor of nine to calculate major areas of the body to add together to sum up burn extent. Below are examples of how adults and pediatric patients are assessed:
If you add up all the values on the adult, they are 100. The numbers on the limbs and head are circumferential, so if only the front of someone is burned, those numbers are halved.
Note that the numbers shift on the pediatric patient to 18% for the head and 14% for the legs. This accounts for the fact that children have proportionally larger heads than adults, so any burns to head are going to be more surface area.
Rule of palms – this is handy – no pun intended – for measuring smaller burn areas. Look at the size of your patient’s palm and find some way to use an analog measuring device for it. Place the “palm” area on the burn area and add up how many “palms” the surface of the burn area is. Each “palm” is approximately 1% of the patient’s body surface area. So if you have five “palms,” the patient has a 5% BSA burn.
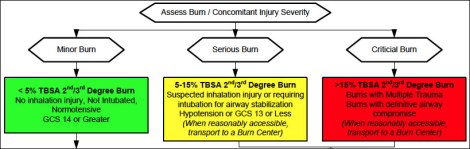
Once you have %BSA and the thickness of the burn area quantified, here is a handy chart for determining the severity of the patient’s injuries. Please note that there are some body areas, like face, hands, feet, and genitalia, that make for an automatic critical burn because of the location, regardless of the %BSA.
Below are the American Burn Association’s criteria for referring a patient to a burn center for treatment.
1. Partial thickness burns greater than 10% total body surface area (TBSA).
2. Burns that involve the face, hands, feet, genitalia, perineum, or major joints.
3. Third degree burns in any age group.
4. Electrical burns, including lightning injury.
5. Chemical burns.
6. Inhalation injury.
7. Burn injury in patients with preexisting medical disorders that could complicate management, prolong recovery, or affect mortality.
8. Any patient with burns and concomitant trauma (such as fractures) in which the burn injury poses the greatest risk of morbidity or mortality. In such cases, if the trauma poses the greater immediate risk, the patient may be initially stabilized in a trauma center before being transferred to a burn unit. Physician judgment will be necessary in such situations and should be in concert with the regional medical control plan and triage protocols.
9. Burned children in hospitals without qualified personnel or equipment for the care of children.
10. Burn injury in patients who will require special social, emotional, or rehabilitative intervention.[4]
Grid up treatment
Burns are trauma – so do your good trauma assessment and don’t be freaked out by the burns. You don’t want to miss something that is going to kill your patient because you are focused on the thing most obvious. If your patient fell into a bonfire because he’s stroking out, you’d better be able to find that out fast and treat what’s going to kill him first. Burns are ugly and painful, but they can be distracting injuries.
Don the best PPE you can find and get ready to go to work. Ideally, you’ll be in SCBA (Self-Contained Breathing Apparatus) gear, Nomex, insulated boots, and leather or Nomex gloves. Ideally.
For chemicals, you may need SCBA and a Tyvek. For radiation, I hope you have a robot and full HazMat setup with decon.
Your safety has to be paramount, because a bad response can turn a bad situation into a catastrophe if responders start becoming casualties.
Once you encounter any kind of burn patient, the first order of business is to get him out of the environment where he is being burned. If his clothes are on fire or smoldering, get him out of those and to safety.
If it’s a suspected chemical burn, brush off dry chemicals (with something other than your hands), get the patient out of his clothes and to safety. Be careful to not contaminate yourself. Use as much PPE as you can get your hands on to protect yourself from whatever toxins are injuring your patient. Irrigate when appropriate.
If it’s an electrical burn, get the patient out of that situation, check for burning or smoldering clothes, get him out of those, and get him to safety. Take LOTS of care to assess this scene and understand where the current is flowing. Find the source of electricity and kill the power if you can. Look for water on the ground or the ceiling that might be dripping down. Look for wires. Use insulated tools to pull the patient out. You DON’T want to get electrocuted yourself. It would be very bad.
If it’s a radiological injury, you might want to eat a bunch of potassium iodide (KI) pills, don a lead suit, cup your testicles, and get the patient out of the situation to decon and treatment. Hopefully you’ll know if the radiation is alpha, beta, or gamma ray. If it’s gamma ray and you’re standing next to the patient, been nice knowing you, Dr. Bruce Banner.
Now – I am sure my Hook and Ladder, HazMat, and USAR guys are grousing because I essentially just killed a bunch people by having them rescue a burning patient without knowing squat about TTPs for search, rescue, and HazMat ops. You are correct.
In an ideal world, there would be an Incident Command Structure, an Incident Commander, Section Chiefs, hot, warm, and cold zones, decon, triage and treatment areas, and a bevy of other awesome things that mitigate crew risk and maximize patient care. However, this is grid down medicine, where “life sucks, improvise” is the order of the day, so you do what you can. If anyone with Fire Rescue, HazMat, and / or USAR experience would like to chew on a grid down version of your area of expertise, Brother (or Sister), we are all ears and would love you to drop your science in a post one day. Hats off to you all for doing some hard work.
Let’s get back on task.
Thermal burn treatment
Once the patient is removed from the burning environment, as stated earlier, get that rapid trauma assessment in high gear.
Let’s talk about airway for a minute. With burns, suspected inhalation injury needs to be a top priority. If your patient was in an enclosed space of any kind, suspect that he inhaled lots of superheated gases full of poison and soot into his nose, mouth, larynx, trachea, and lungs. If you see soot around his face, nostrils, and mouth, you assume the airway is full of the same and will be welding itself shut imminently, even if he is asymptomatic at the moment. If your patient wasn’t in a sealed space but has burns on the upper body, expect all the same.
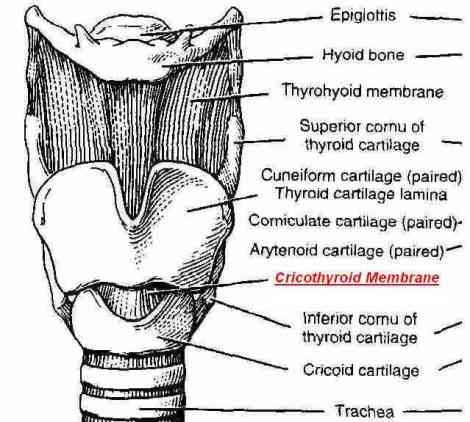
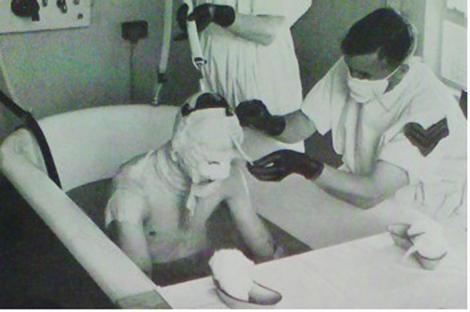
Keep an eye and ear out for stridor, wheezing, hoarseness, coughing, and anything else that can think of that would indicate airway compromise. If your patient’s face is already swollen you are in really deep doo-doo and may need to start thinking about a surgical cricothyrotomy. The photo below shows a burn patient that has a tracheotomy evidenced by the swelling in his mouth, a nasogastric tube, and the ventilator tubes that are attached to a point in his neck. Tough day for this man.
Clinical note: advanced procedures ahead. Be sure you know what you are doing here. Burned, swollen airways are automatically difficult airways, this is not rookie stuff.
Get on the ball to do a prophylactic advanced airway. One option is rapid sequence induction (RSI) and an endotracheal tube. If you are going with RSI, be careful with succinylcholine and intracellular potassium being extracellular potassium (hyperkalemia) thanks to cell damage and / or fluid shift. The general consensus is that you have a 72-hour window after the initial burn to use succinylcholine. The other major issue with RSI is that you take away the patient’s ability to breathe for himself. If you have a ventilator ready, that’s great, if not, you’ll need a couple of people around to run a bag-valve mask and ventilate the patient until he can be ventilated.
Nasotracheal airways are a decent alternative if you have no good sedation drugs. Paramount is that the patient must be breathing on his own, because you insert the NT tube through the nare and snake it down the back of the nasopharynx and oropharynx and into the trachea upon inhalation. Synch with the patient’s breathing and when he inhales, push it further in the trachea. Confirm placement using lung sounds, chest rise and fall, condensation in the tube and colormetric ETCO2 or capnography if you’ve got it. It’s not pretty or comfortable for your patient, but it works. In the video above, you can see the patient coughing and bucking once the NT tube was placed. This is an unfortunate side effect of the NT tube that can possibly be mitigated with lidocaine injected through the cricothyroid membrane. Below is a video of an anesthesiologist that performs a conscious endotracheal intubation on himself. Start at 1:22 for the good stuff.
This is a case where it’s better to have a tube and not need it, than to need a tube and be unable to get it. Back to our regular programming.
[Grouch adds: If I have a slightest hint of possible airway burn and I don’t get a tube down that trachea, I have royally F’d up. If I miss that in my clinical practice, it is more than an open-and-shut malpractice case, it’s a “should we even let this fool keep his license?” situation. Get the freaking airway.]
As you are assessing the airway, make sure someone is helping stabilize the patient’s cervical spine. Again – burns are trauma, so do what you’d normally with a trauma patient.
Continue the rapid trauma assessment (ABCDE) and fix any life threats. As you go about your assessment, remove any constricting articles from the patient like rings or watches that could cause circulatory compromise as the patient swells from his burns.
Get 100% high-flow oxygen going as soon as the airway is established. 15 liters per minute. The important thing here is to assume that the patient probably has some level of carbon monoxide (CO) poisoning if not cyanide (CN) poisoning as well. Pulse oximetry is unreliable in a burn patient because CO has an affinity 250 times greater for hemoglobin than oxygen and will return a false high O2 saturation reading on the pulse oximetry sensor. You need to get the high flow O2 going to jump onto any hemoglobin that hasn’t already combined with CO.
Since we are grid up, our goal is to get the patient to definitive care. To that end, in the pre-hospital setting, that means rapid transport. Get him packaged and moving quickly.
Remember the Trauma Triangle of Death: Acidosis, Coagulopathy, and Hypothermia. Your burn patient is trying to do all three at once, so the initial resuscitation needs to be pretty aggressive.
A critical step in the treatment of a burn patient is fluid resuscitation. As mentioned above, the fluid shift phase happens over the first 24 hours after the burn, and it is important that the patient receives fluid to keep his organ systems perfused.
Start two large bore (18 gauge and lower) IVs through unburned skin if available. If not, through burned skin or intraosseous is acceptable. Now it’s time for med math.
The most commonly used method for calculating fluid needs for a patient is called the Parkland Formula, and with it, you calculate how much fluid the patient will need in the first 24 hours after the burn. You take the total volume of fluid, and give half in the first 8 hours and the other half in the remaining 16 hours. This level of fluid resuscitation is generally not required for superficial burns.
The Parkland formula: 4mL of fluid per patient weight in kilograms x the %BSA burned.
For example, if our patient weighed 100kg and had a 36% BSA burned, the formula would look like this.
4mL x 100kg x 36 = 14,400mL of fluid over 24 hours. 7,200mL will be given in the first 8 hours and 7,200mL will be given in the remaining 16 hours.
The preferred fluid is Lactated Ringer’s because of its electrolyte mix, its buffering properties once metabolized, and that it has a closer-to-neutral pH than 0.9% normal saline. Still, saline will keep a patient alive and it’s not the end of the world if it’s all you have to work with.
Those not experienced with burns look at that amount of fluid and balk. It’s typically a TON of fluid, compared to almost any other situation in medicine. However, patients that do not receive adequate fluid resuscitation have very poor outcomes, so its very important to get this going quickly. Always be on guard for pulmonary edema from fluid overload, but if you have taken control of the airway, it’s more important to get the fluid in (within reason). Keep listening to lung sounds as you transport.
Next, you’ll need to wrap the patient in a clean dry sheet and guard against hypothermia. Whatever you are transporting in, turn the heater on and get it warm where the patient is. If you are sweating and uncomfortable, then the temperature is just about right.
Burn patients are going to be in a lot of pain. Grid up means morphine IV and lots of it. Remember that morphine depresses the respiratory drive, so keep on eye on your patient’s breathing. Get a SAMPLE history to make sure your patient isn’t allergic to it. If he’s unresponsive, pray he isn’t allergic and have anaphylaxis supplies ready, just in case.
If you’ve done all of these things, you are pretty much done with the pre-hospital portion of a burn patient in the grid up world. Reassess every five minutes all the way to the hospital. Call Medical Control for more morphine if it’s a long transport, and call a supervisor to meet you somewhere in route with more. Keep burn patients as comfortable as can safely be done.
At the hospital
I will touch on as much as I can here, but I am a little out of my lane so I am going to remain general. Burn care is very complex and breaks many of the well-established rules of thumb in other fields of medicine. Any of you guys that do this for a living are welcome to drive out more detailed information in the comments.
Once at the trauma center or burn center, the patient will undergo all sorts of extra monitoring and specialized care, but it still starts with a trauma assessment by the staff. ABCDE all over again.
If the patient has circumferential burns around the chest, he will most likely receive a thoracic escharotomy because the damaged skin around his chest will not stretch and allow for adequate breathing. The eschartomy is a series on incisions made at key points on the body that will allow for adequate breathing and circulation in the extremities. The incisions go through the epidermis and dermis down to the subcutaneous fat layer. Anything deeper than that and the escharotomy becomes a fasciotomy, because you are now cutting into muscle, and there are a whole new range of concerns with that. A simple guide on an escharotomy is to cut until pink. If you cut into black and it’s still black at the cut line, you need to go a little deeper.
Below is a diagram of where the cuts take place in an escharotomy.
Source: https://sydneyhems.com/
Here’s what one looks like in real life.
Once the ABCs are stable, the patient will probably get a nasogastric (NG) tube to evacuate the stomach to keep intraabdominal pressure down and to mitigate an intestinal blockage or paralysis, called an ileus, which can be caused by severe burns. A Foley catheter will be inserted in the urethra / bladder to monitor urinary output, which should be about 25 – 50mL/hr in adults and 1mL/kg/hr in pediatric patients.
More advanced monitoring will be set up, and may include
-
Pulse oximetry and CO-oximetry
-
Arterial blood gases (ABGs)
-
Carboxyhemoglobin level
-
Lactate
-
Complete blood cell count (CBC)
-
Chest radiography
-
Electrocardiogram
-
Serial cardiac enzymes (in patients with chest pain)
-
Pulmonary function testing
-
Direct Laryngoscopy and fiberoptic bronchoscopy[5]
- Cyanide levels
A high lactate level in a burn patient can indicate the level of cyanide toxicity the patient may have from smoke inhalation.[6]
The patient may be fluid resuscitated for approximately 48 hours, during the second 24 hours, a colloid like albumin may be titrated in with the Lactated Ringer’s or saline. During this process, all circumferential partial and full thickness burns will be monitored for edema causing compartment syndrome under the skin. If pulses in the distal extremities become faint to absent, extremity escharotomy may be indicated to restore circulation.
Wound care starts in the hospital and includes cooling, irrigation, cleaning, and debridement of the burn. Burns require regular cleaning, application of burn creams like silver sulfadiazine, and fresh, non-adhesive dressings. This is all done with copious amounts of narcotics and sometimes sedatives / anesthetics like midazolam or ketamine to keep the patient comfortable and calm.
Since burns destroy our physical barrier of protection against microbes, much attention is paid to stave off infections with antibiotics. Excellent wound care, infection control, nutrition, and monitoring are critical to a good outcome.
As the patient moves from the fluid shift phase into the hypermetabolic phase, he is going to need lots of extra nutrition and protein. In order to repair the burns, the body will consume itself, namely fat and muscle, to keep itself alive, so those extra calories are going to help prevent muscle loss as the patient heals.
The burn team is typically a surgical team, as most burns (especially full thickness burns) are treated with a series of surgical operations, which can include skin grafts, eschar excisions, fasciotomies, debridements, and etc.
From there on out, it’s more of the same with the goal of starting rehabilitation and getting the patient back to as normal of a life as he’s going to get. Anyone that has been severely burned has experienced a life-changing event that will require years – if not a lifetime – of support from his care team, family, and friends.
Chemical burn treatment
A chemical burn is an automatic HazMat scene. As mentioned earlier, HazMat response TTPs are not covered here, so we are ASSUMING that the patient got the full HazMat treatment, and is cold, wet, and naked in your truck because the offending agent has been removed from him. If he is not, then he needs to get a poor-man’s decon of dry-brushing off the offending agent and removing any clothes that are saturated and causing the burn. Make sure to seal the cut clothes into a biohazard bag and put the bag in an exterior compartment of the truck away from the crew and patient compartments. Call your supervisor for the best way to dispose of the bag, because there may be different protocols for HazMat than biohazard. Irrigate the wound with sterile water, but don’t take all day. Rapid transport to definitive care.
In pre-hospital, you treat this patient the same way you treat a thermal burn patient. ABCDE trauma assessment, battle back the Trauma Triangle of Death.
Be sure to use extra PPE and monitor yourselves for and signs and symptoms that indicate whatever toxic substance harmed the patient is not floating around your truck and being inhaled by your crew. If you do see signs of toxicity, then stop the truck, open the door, and get the patient out. Call the HazMat team when you do, but Do Not repeat DO NOT make yourself sick. This sounds cruel, but your first priority must be your own safety.
At the hospital
Generally, the chemical burn patient is going to have his burn irrigated – or lavaged – with water for a while. If it’s an acid burn, it will be shorter in duration. If it’s an alkali burn, it may be much, much longer in duration.
Once the burn team is happy with the level of lavage and neutralization of the offending agent, then the treatment will be generally the same as a thermal burn patient.
Electrical burn treatment
Electrical burns are a special breed, because they cause all sorts of damage that can’t be seen. Most of the time you will see entry and exit wounds, but understand that the path the electricity took through the patients body damaged organs, muscles, nerves, and blood vessels. The video below gives you an idea of the kinds of forces we’re dealing with. Remember, the energy you see is also going through the inside of this hapless man’s body. GORE WARNING.
http://www.liveleak.com/ll_embed?f=a937c4424a1f
In the pre-hospital setting, once the scene is safe and the patient and responders are out of danger, the treatment for the patient is a combination trauma and cardiac patient. If he is unresponsive, suspect cardiac arrhythmia induced by the electric shock. Take c-spine precautions, get the patient on the cardiac monitor and treat as per BCLS / ACLS protocols. If there is return of spontaneous circulation, conduct a rapid trauma assessment, package the patient in full spinal immobilization and transport rapidly.
If he is breathing and has a palpable carotid pulse, follow the same pre-hospital treatment plan for thermal burns but with advanced cardiac monitoring.
Whatever the case, it is import to get some kind of report from the scene get the mechanism of injury. If the patient had an electrical contact and “couldn’t let go” then he most likely contacted alternating current (AC). If the electrical contact caused the patient to be “blown back” from the point of contact, he most likely contacted direct current (DC). The AC current will cause rapid muscle contractions that make it impossible for the patient to relax or let go of the contact. The DC current will cause one violent convulsion. In either case, be highly suspicious of neck and spinal injury. Knowing the voltage, current, and duration of the contact are key pieces of information to pass on to the clinicians at the hospital.
A lightning strike patient should be treated the same as any other electrical burn patient. While the electrical energy that goes through the patient is very large, the duration is extremely short, which may explain why there are lots of lightning strike victims that have lived to tell about it. A telltale sign of a lightning strike is a treelike scar pattern on the skin called a Lichtenberg figure.
In the hospital
The treatment of electrical burns in the hospital differs from thermal burns because of the damage done to the muscles, organs, and other tissues inside the body. In addition to the thermal treatment protocols, there is a great concern for damaged tissues, especially muscles, releasing massive amounts of proteins into the blood, that will literally clog the kidneys. Dark or tea-colored urine (myoglobinuria) or blood in the urine can be signs of this, making fluid resuscitation all the more critical for these patients. Increasing the resuscitation to yield 2mL/kg/hr of urine may be required.
Compartment syndrome is another concern, so peripheral pulses need to be continuously monitored. If pulses are lost and compartment syndrome is suspected, escharotomy or fasciotomy of the affected limbs may be required.
Radiation injury treatment
When the grid is up, you’re pretty much going to know where the risks of radiation exposure are thanks to things like the National Fire Protection Association’s NFPA 704: Standard System for the Identification of the Hazards of Materials for Emergency Response placards or USDOT hazardous materials placards that let you know that something radioactive lurks in a vehicle or building. These systems are designed to let responders know the nature of the hazardous materials they may encounter in a fire.
People who work in environments where radioactive materials are present are usually required to wear dosimeters and pass through radiation detectors when they leave work. This can be military sites, nuclear power plants, nuclear medicine facilities, research labs, etc.
The thing about radiation, is that it is particles – as described above – that are the sources of radiation. These particles end up on people, people’s clothes, and all the gear they have with them. So to that end, the first thing to do when there is some kind of radiation incident is to isolate and contain the source, then isolate and contain the people and stuff that were exposed. Decon requires that the exposed people be stripped of all of their clothes and then be washed in soap and water – not abraded – and then they can start to be treated for exposure.
You want to be on the lookout for the signs and symptoms of Acute Radiation Syndrome.
The required conditions for Acute Radiation Syndrome (ARS) are:
- The radiation dose must be large (i.e., greater than 0.7 Gray (Gy)1, 2 or 70 rads).
- Mild symptoms may be observed with doses as low as 0.3 Gy or 30 rads.
- The dose usually must be external ( i.e., the source of radiation is outside of the patient’s body).
- Radioactive materials deposited inside the body have produced some ARS effects only in extremely rare cases.
- The radiation must be penetrating (i.e., able to reach the internal organs).
- High energy X-rays, gamma rays, and neutrons are penetrating radiations.
- The entire body (or a significant portion of it) must have received the dose3.
- Most radiation injuries are local, frequently involving the hands, and these local injuries seldom cause classical signs of ARS.
- The dose must have been delivered in a short time (usually a matter of minutes).
- Fractionated doses are often used in radiation therapy, and are typically in the range of 0.5-0.7 Gray (which is the toxic dose mentioned above) divided up over a 7 week course. Fractionated doses are less effective at inducing ARS than a single dose of the same magnitude.
The three classic ARS Syndromes are:
- Bone marrow syndrome (sometimes referred to as hematopoietic syndrome) the full syndrome will usually occur with a dose between 0.7 and 10 Gy (70 – 1000 rads) though mild symptoms may occur as low as 0.3 Gy or 30 rads4.
- The survival rate of patients with this syndrome decreases with increasing dose. The primary cause of death is the destruction of the bone marrow, resulting in infection and hemorrhage.
- Gastrointestinal (GI) syndrome: the full syndrome will usually occur with a dose greater than approximately 10 Gy (1000 rads) although some symptoms may occur as low as 6 Gy or 600 rads.
- Survival is extremely unlikely with this syndrome. Destructive and irreparable changes in the GI tract and bone marrow usually cause infection, dehydration, and electrolyte imbalance. Death usually occurs within 2 weeks.
- Cardiovascular (CV)/ Central Nervous System (CNS) syndrome: the full syndrome will usually occur with a dose greater than approximately 50 Gy (5000 rads) although some symptoms may occur as low as 20 Gy or 2000 rads.
- Death occurs within 3 days. Death likely is due to collapse of the circulatory system as well as increased pressure in the confining cranial vault as the result of increased fluid content caused by edema, vasculitis, and meningitis.
The four stages of ARS are:
-
Prodromal stage (N-V-D stage): The classic symptoms for this stage are nausea, vomiting, as well as anorexia and possibly diarrhea (depending on dose), which occur from minutes to days following exposure. The symptoms may last (episodically) for minutes up to several days.
-
Latent stage: In this stage, the patient looks and feels generally healthy for a few hours or even up to a few weeks.
-
Manifest illness stage: In this stage the symptoms depend on the specific syndrome (see Table 1) and last from hours up to several months.
-
Recovery or death: Most patients who do not recover will die within several months of exposure. The recovery process lasts from several weeks up to two years.[7]
In a pre-hospital after the patient is decon’d, the job is primarily supportive care and treating symptoms like nausea, vomiting, and headache. There may be some redness of the skin where the exposure took place, but in terms of burn care, there may be very little unless the patient was exposed to a thermal AND radioactive substance, like high-pressure steam or a nuclear bomb blast.
In the hospital
Depending on the dose of the exposure and severity of ARS, care will again be supportive and symptom-based. Fluids, electrolytes, blood products, antibiotics, and fever control. If the patient is expectant, then it will be comfort measures.
Grid down treatment
FINALLY, we get to the fun stuff. Gentle reminder that if the grid is up, don’t use these as substitutes for available medical care. No doctor in his right mind takes care of a burn patient outside of a dedicated burn center. Doc Grouch has personally sent a critically ill patient to a burn center located on the other side of Texas, to give you some idea of the high priority given to burn centers in the medical community. There is a lot not to like about the financial aspects of our medical system, but the care you get from people who love what they do with the world’s best technology is always going to be better than practicing ditch medicine at home. Not everything in here is perfect, sterile, and risk-free. It’s grid down and life is hard, so we do the best with what we have. We will make some assumptions here, in that the grid down medical clinic will have some basic things like water, basic sanitation, a source of heat, a pressure cooker for sterilization, and some basic medical supplies. What we won’t have is lots of electricity, high end monitoring equipment, and a fully-stocked hospital pharmacy.
Everything already covered in grid up treatment still applies. However, we may not have a burn center, less a trauma center, or even a community hospital to take the patient to.
We’re still going to need an airway, adequate breathing, circulation, and fluid resuscitation.
Doc Grouch’s post on improvised laryngoscopes is a great starter for finding ways to visualize airways. The bent spoon with a commercial fiberoptic camera is a great example. If you have ET tubes, awesome. If not, here’s where the creativity begins.
If the airway is bad, there is the hollow pen body through the cricothyroid membrane method. This is about as temporary as you can get as the hollow pen body is not wide enough for sustained oxygenation and ventilation. What it does is buy you time to try and get a full cricothyrotomy or tracheotomy done with a larger breathing tube.
In austere conditions, a tube is a tube is a tube, and you can adapt chest tubes, Foley catheters, and other medical tubing to perform as temporary airways. If there’s no medical tubing, find any kind of tube and clean it. If you can sterilize it in a pressure cooker, bully for you. Just use it to buy time to get a better airway later. Try not to use the fuel hose from the village garbage truck, though.
Breathing gets a little complicated because we’re austere, and we’re going to need a small army of people to run a bag valve mask in rotation, if that’s all we have. If things are limited, an oxygen concentrator can pull nitrogen out of room and air and supply some form of oxygen. It doesn’t require a lot of electricity to run and it certainly could help. Pa4ortho and Doc Grouch had some banter back on our shock post, where they discuss some improvised systems for longer-term patient ventilation. Also, BOLO for a post on ventilators and their improvisation soon.
In off grid medicine O2 seems to be first thing to get discarded due to wt and logistic burden, as well as low efficacy in making a difference in general trauma. I try to save it for HAPE/HACE [high-altitude pulmonary edema / high-altitude cerebral edema] or pulmonary injury. Just what I do.
At my definitive off grid Tx facility I have a O2 concentrator on battery and solar power that is part of the drawover anesthesia set up.
I can be used for a Respiratory patient but is limited to 4 liters per minute.
CPAP and O2 potentially could be a big deal in managing respiratory complications of viral illness.
Poor mans low tech vent.
Both are low power enough to run on solar.What are your thoughts? It’s your specialty. I’m always looking for input.
Viral, bacterial, inflammatory…the list goes on.
Found this:
http://www.secondwindcpap.com
that is an old RT selling used cpap or bipap machines for substantially less than new.
That and an old oxygen concentrator would go a long way.
In the old days they hand-ventilated patients using something very similar to an ambu bag. I’d think that would be difficult without lots of manpower.
The uninterrupted power supply would be difficult, and there is a limit to how much you can do with typical portable O2 concentrators. But you would save some folks, no doubt.
Will think on this further.For long term bagging a patient put a foot operated zodiac pump on the circuit block the travel of the pump to prevent too much tidal volume. Set up with a reclining chair like a leg press machine at the gym.
Circulation requires some form of IV or intraosseous access, especially for fluid resuscitation if your patient has a burn greater than 20% BSA. Again, it’s Lactated Ringer’s preferred before 0.9% normal saline.
If you have a patient with no airway compromise, is alert, can swallow, and has less than 20% BSA burned, listen intently to the patient’s abdomen for sounds that indicate his gut is still working and that ileus we mentioned earlier is not an issue, he may be eligible for rehydration orally. This is only recommended if you have no better options, because you need to be very cautious about the ileus. Mix up some oral rehydration solution and get to work. This is better than nothing. You do everything you can with what you have.
Ideally the recipe is:
- 1L water
- 20g glucose
- 3.5g salt
- 5g baking soda (sodium bicarbonate)
- 1.5g potassium chloride
If all you have is water, salt and sugar, then the recipe is:
- 1L water
- 8tsp sugar
- 1tsp salt
In adults, we’re hoping for urine output of .5mL/kg/hr and 1mL/kg/hr in pediatrics.
Pain control will be complicated. Controlled narcotics and sedatives may be tough to get. Administration of over the counter pain meds like Ibuprofen and Tylenol may be the best you can do.
For those jumping up and down yelling “I can just grow opium poppies!”, yes, that’s true. You can find extensive documentation on the web regarding growth and harvesting of the active substance. Please, for the sake of sanity, do not experiment with this stuff prior to a true grid-down emergency. Regardless of your opinion of the drug laws, the SWAT team still takes a dim view of homemade heroin. No need to borrow trouble.
Antibiotics will likely be in short supply, so focusing on sanitation, infection control, and disciplined wound care will be very important.
There are multiple options for wound care. They all follow a simple philosophy of assess, cool the burn, control pain, clean, treat, dress and repeat. When possible, elevate burned extremities above the level of the heart to keep swelling at a minimum. This may help avoid compartment syndrome and the need for escharotomy or fasciotomy.
A handy temporary measure – and if you can get the patient to definitive care like a burn center – is after cooling and irrigating the burned area, applying Saran Wrap. It has to be tiled and not wrapped circumferentially, as it may limit circulation and movement. This will not adhere to the wound surface and also keeps air from blowing on the burned area, mitigating some pain. It is important that the wrap covers an ample margin of unburned skin next to the burned area. This is not recommended for more than six hours.[8]
You can cool the burn by placing wet towels or sheets covered with dry towels on the burn. Watch for hypothermia when doing this. Once cooled, cover the burn with silver sulfadiazine, antibiotic ointment, or even Manuka honey (discussed further down), then place clean, dry dressings on the burned area. NEVER pull off a dressing that has fused onto a burn. Soak the area with half-strength saline until the dressings come off. This may take hours.
Burned hands and feet can be put in plastic bags that have liberal amounts of burn cream or antibiotic ointment in them. Make sure there is enough room in the bag for the extremity to move around freely. Encourage the patient to move it around. Create a collar at the bag opening around the leg or arm with gauze and tape to seal the bag. Don’t make it too tight as to compromise circulation. Keep the limb elevated. The important thing is that the inside of the bag should be moist. Assess, clean, and rebag the wound daily.
For partial thickness burns, the exposure method has the patient kept in a room at 104F and humidity controlled to greater than 39%. The room has to be airy and the patient beds need to have at least 5 feet of space between them. The burns need to be cleaned and then the patient placed on a sterile sheet on the bed. A “burn tent” composed of another sterile sheet would be placed over the patient on the bed. The key is to not have the top sheet touch the patient’s burns. Think back to the old GI half-shelter. Pitch one on a patient’s bed with some wire, or paracord, and you’re good to go. The patient will need to be monitored and appropriately medicated as his wounds heal.
If you have electricity, a household iron can be a way to sterilize sheets by simply ironing them.
Full thickness burns can use a saline treatment method, where half-strength saline or boiled seawater is used to moisten gauze placed over the burns. The gauze needs to be changed daily. Hypothermia must be monitored for at all times with this method. This is another one where a very warm room is ideal. You can also soak a full thickness burn in a tub full of water that has 1 teaspoon salt and 1/2 teaspoon of bleach per liter of water. The water will need to be changed daily and the vessel will need to be cleaned and scrubbed with detergent daily as well.
In both the exposure and saline method, debridement needs to happen daily, but can be done by having the patient and his caregivers simply bathe in soap and water. It is important that necrotic tissue is removed regularly to stave off infection. This also means ample use of pain meds. Showers are preferred because they are cleaner. If a bath basin is all you have, drain the water and clean it after each patient to avoid cross-contamination.
“Debridement” and “ample use of pain meds” sounds very cut and dried, but can be one of the most emotionally traumatic things that burn teams do. They sometimes cannot give enough meds to keep the patient out of pain. They have to dress in such a way as to conceal their identity so the patient will not be frightened of them later. And the team itself can have bad PTSD because they feel more like torturers than healers. Methods have improved in modern times, but by definition you won’t have those in a grid-down scenario. This won’t be easy on anyone.
Burns on the eyes and eyelids are complicated and a big concern. Superficial burns of the cornea can heal with the help of lots of antibiotic ointment or drops directly in the eye. Deep corneal burns most likely will result in surgery and loss of the eye. If the eyelids are burned, the protocol is the same to clean the burns, apply ointment, moist dressings, and try to have the patient keep his eyes closed. These burns require some of the most specialized care that can offered in a grid up world. In a grid down world, these will be very challenging.
A grim but effective burn dressing is actually a body bag. It retains moisture, has a smooth interior, and has handles that make for easy patient carrying. These would be used for pretty large %BSA burns, and in grid down, the prognosis for burns that size will be poor. Keep these patients intubated, sedated, and full of pain meds if you can.
Manuka honey has shown some promise in the treatment of burns, as it appears to get the burn sites sterile in less time than silver sulfadiazine. The use of honey follows the wound care methodology of burns. The burned area is cooled, irrigated, and cleaned. Manuka honey is applied in lieu of silver sulfadiazine and gauze dressings on top of those. The cycle is repeated daily. A study showed that patients got out of the hospital faster and with less wound site contamination than silver sulfadiazine.[9] This is a great thing for grid down wound care in general. Regular honey works too, don’t get hung up on the Manuka thing, it’s just what was used in the study. Have a beekeeper friend in your circle of friends or start keeping bees yourself for when the grid goes down.
Be careful putting Vaseline on a fresh burn because it is occlusive, non-sterile, and may cause infection.[10]. However, it can be used further into the wound care process.
Speaking of Vaseline, we will point out an exception to the above rule. In the case of a tar or asphalt burn where the offending agent has fused to the skin, cool the burn, clean around the tar, then put a layer of Vaseline or mineral oil on the tar and apply a dressing. Check it daily and gently wipe the tar away. If more remains, repeat the process until it is gone and then treat the burn as you normally would treat a thermal burn.
Infection
You don’t want to do prophylactic IV or oral antibiotic treatment initially on a burn patient. Topical antibiotics/antiseptics (such as the silver sulfadiazine) are good from the outset. Go through the initial phases of wound care and assess all the burns. Patients are going to get febrile, tachycardic, tachypneic, and have weird blood pressures when they transition from the fluid shift phase to the hypermetabolic phase, so don’t assume right away there is an infection or sepsis. Check the zone of hyperemia and note if it is expanding over time. Standard grid up care is not to give antibiotics to infected burn wounds–instead, the newly infected area is surgically removed. Antibiotics are reserved for patients in septic shock. If blisters are filling with cloudy fluid and the wounds begin to smell, then aggressive debridement is needed. If the patient starts dropping their blood pressure, gets tachycardic, and has bacteria visible in their blood smears, then consider broad-spectrum antibiotics. Unfortunately, most truly broad spectrum antibiotics are IV only; if you have plentiful access to those you likely don’t need our advice. Vancomycin, Zosyn, Meropenem, daptomycin and the like are all used. Watch out for the development of resistant bacteria. If you are limited to oral medications, things like augmentin, doxycycline, bactrim, cipro or its cousins, will be the mainstay. Without a lab to tell you what bacteria are present you will be shooting blindly, so you will have to give more than one drug. Given the above limitations, excellent wound care and infection control procedures are your friend.
Now if your burn patient comes into the clinic with traumatic amputations and / or huge lacerations full of asphalt, dirt, and viscera from livestock and people, then yes, treat with prophylactic antibiotics.
Grafts
Grafting skin is very serious business and ideally should be done by an advanced clinician – PA, NP, MD, etc. Grafts should be done on skin affected by full thickness burns. The skin needs to be free of eschar and infection, should be pink, and bleed easily. The donor site should be free of infection – like zits – and should match as closely as possible to the skin it is replacing. You don’t want hairy thigh skin replacing forehead skin, unless you don’t like the guy you’re fixing. In grid down, don’t get grafts from other donors. You’ll be playing an immune system game you don’t want to start. If you’d like to learn more about how to do grafts, we’d recommend reading many of the reference books listed below and getting some training under someone that has done it.
Physical therapy
As soon as possible, a burn patient needs to be moving affected joints and limbs to maintain and regain as much mobility as possible. As can be imagined, moving around burned and healing limbs is going to hurt like hell, so adequate pain control is going to be critical to make this happen. Even if it’s passive movement by a caregiver, anything is better than nothing. Limbs that are burned so badly that they are flexed into abnormal positions may need to be splinted. Care must be taken to wrap individual digits in burn cream and dressings to avoid fusing.

Avoid this if possible.
Source: http://www.ijps.org/article.asp?issn=0970-0358;year=2010;volume=43;issue=3;spage=72;epage=79;aulast=Sabapathy
Make your own silver sulfadiazine
The following recipe for silver sulfadiazine for all you would-be chemists out there comes from a great book that’s tough to find from David A. K. Watters, et al., called, Care of Critically Ill Patient in the Tropics and Sub-tropics. It’s an excellent book and written to help people function medically in grid down environments.
Make and use at your own risk.
Reagents
Sulphadiazine (or sulphadimidine) 146 500-mg tablets.
Silver nitrate crystals 48.5 g.
Sodium hydroxide pellets 11.5 g.
Glycerine 1440 ml.
Liquid paraffin 560 ml.
Non-ionic emulsifying wax 1100 g.
Hibitane solution (leI), 5% 320 ml.
Sterile distilled water as required.
Instruments
A 10 liter bucket, a mixer, a mixing rod, a beaker, and a heater.
Method
Dissolve the sodium hydroxide in about 100 ml of water. Dissolve the silver nitrate in 4000 ml of water.
Suspend the sulphadiazine tablets in 1000 ml water and stir. Heat to boiling point and add to the suspension the solution of sodium hydroxide while stirring. Slowly add the solution of silver nitrate to the suspension of sulphadimidine and sodium hydroxide. A white precipitate of silver sulphadiazine will form. Stop adding silver nitrate when a brown precipitate of silver oxide shows that the formation of silver sulphadiazine is complete. Boil for some minutes to make the precipitate finer and more easily filterable.
Separate the precipitate: (1) by centrifugation, or (2) with an old glass filter, or (3) by letting it stand overnight, and pouring off the supernatant. Wash the precipitate many times with water until you can detect no more silver ions in the supernatant.
Mix together the glycerine, the liquid paraffin and the emulsifying wax, and sterilize at 150°C for an hour. Let them cool and add the Hibitane solution warmed to 80 0c. Mix the 2 preparations and stir vigorously to obtain a fine pink cream. Put the bucket into cold water and mix until cold. Meanwhile add enough distilled water to bring the volume up to 8 litres before the preparation becomes cold.
In closing
Burns are a complex form of wound that affect many systems at once, and they best way to treat them is to understand the underlying physiological processes that a burn patient will go through from initial contact to full recovery. In a grid down scenario where supplies and trained personnel are limited, a person that suffers 50% or more BSA partial and / or full thickness burns would probably get palliative care whereas rapid transport to a fully staffed and stocked burn center gives him a much greater chance of survival. Triaging burn patients will be a hard decision, but you need to focusing on helping the most people you can when your resources are limited.
Education and prevention to avoid getting burns are the best medicine of all. Take the time to think through your plans should the grid go down. If you are using fuels to run generators, always cap off liquid fuel containers immediately after pouring or filling. Know what propane and methane smell like when treated and also that propane is heavier than air while methane is lighter than air in case of leaks. Never underestimate the power of little ones to grab things you thought out of their reach. Know what clothes fabrics are flammable (polypro, nylon, etc.) what ones that are flame resistant (wool, cotton, Nomex, etc.) And please, please, please, please, don’t mess with anything electrical if you aren’t trained to do so.
None of the methods discussed to care for burns in a grid down environment is a guarantee, but they represent a determination not to give up when things go bad. Training and practice are paramount, as well as the ability to improvise with what you have to give your patient the best chance to survive.
Homework
This assignment is very simple. If you have preparations for trying to stay as civilized as possible by using alternate power, heating, and cooking sources during a grid down scenario, please review everything you have and develop a training plan for your family to not only operate these things, but when to stay away from anything that looks hinky, and manage issues should they arise. The proof in the training will come when people have been awake for 24 hours, its dark, everyone’s stressed and scared, but safe in their knowledge in how to avoid getting burned by a generator, stove, electrical wire, or anything else.
Sweat more now, burn less later.
References
1. Rice, Jr, P.L. MD, & Orgill, D.P. MD, PhD. (April 03, 2015). Emergency care of moderate and severe thermal burns in adults. UpToDate®, Retrieved from http://http://www.uptodate.com/store/
2. American Burn Association. (2013). Burn Incidence and Treatment in the United States: 2013 Fact Sheet. Retrieved from http://www.ameriburn.org/resources_factsheet.php
3. List of burn centers in the United States. (n.d.). In Wikipedia online. Retrieved from https://en.wikipedia.org/wiki/List_of_burn_centers_in_the_United_States. (2015).
4. American Burn Association. (2006). Burn Center Referral Criteria. Retrieved from: http://ameriburn.org/BurnCenterReferralCriteria.pdf
5. Lafferty, K. A. M.D. (August 22, 2014). Smoke Inhalation Workup, Approach Considerations. Medscape. Retrieved from: http://emedicine.medscape.com/article/771194-workup#aw2aab6b5b2
6.Frédéric J. Baud, M.D., Patrick Barriot, M.D., Véronique Toffis, Pharm.D., Bruno Riou, M.D., Eric Vicaut, M.D., Ph.D., Yves Lecarpentier, M.D., Ph.D., Raymond Bourdon, Ph.D., Alain Astier, Ph.D., and Chantal Bismuth, M.D. (December 19, 1991). Elevated Blood Cyanide Concentrations in Victims of Smoke Inhalation. New England Journal of Medicine. Retrieved from: http://www.nejm.org/doi/full/10.1056/NEJM199112193252502
7. Centers for Disease Control and Prevention. (October 17, 2014). Acute Radiation Syndrome: A Fact Sheet for Clinicians. Retrieved from: http://www.bt.cdc.gov/radiation/arsphysicianfactsheet.asp
8. Victorian Adult Burns Service. (April 20, 2012). First Aid, Cover the Burn. Burns Management Guidelines. Retrieved from: http://www.vicburns.org.au/first-aid/cover-the-burn.html
9. Gupta, S. S., Singh, O., Bhagel, P.S., Moses, S., Shukla, S., and Mathur, R. K. (2011). Honey Dressing Versus Silver Sulfadiazene Dressing for Wound Healing in Burn Patients: A Retrospective Study. Journal of Cutaneous and Aesthetic Surgery 2011 Sep-Dec; 4(3): 183–187. Retrieved from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3263128/
10. De Souza, B. A. (November 29, 2003). Vaseline and burns. The British Medical Journal. Retrieved from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC286261/
11. US Army Walter Reed Medical Center. (2004). Burns. A. C. Szul, L. B. Davis, (Eds.) Emergency War Surgery. (pp. 28.0 – 28.12). Washington, D.C.: Borden Institute.
12. United States Department of Defense. (2011). Chemical, Biological, and Radiation Injuries: Radiation Injury. COL W. D. Farr, M.C., US Army & CDR L. H. Fenton, M.C., US Navy (Ret.) (Eds.) Special Operations Forces Medical Handbook (2nd Ed.). (pp. 6-53 – 6-54). Skyhorse Publishing
13. United States Department of Defense. (2011). Burns, Blast, Lightning, & Electrical Injuries. COL W. D. Farr, M.C., US Army & CDR L. H. Fenton, M.C., US Navy (Ret.) (Eds.) Special Operations Forces Medical Handbook (2nd Ed.). (pp. 7-17 – 7-27). Skyhorse Publishing
14. Bledsoe, B.E., Porter, R.S., Cherry, R.A. (2009). Burns. Paramedic Care, Principles and Practice, Trauma Emergencies (pp. 182-220). Upper Saddle River, NJ: Pearson Prentice Hall
15. Iverson, K. V. M.D., M.B.A., F.A.C.E.P., F.A.A.E.M. (2012). Airway, Burns. Improvised Medicine. (pp. 83 – 93), (pp. 337 – 345). McGraw Hill Medical
16. Vanderkooi, M. M.D., D.T.M .& H. (June 20, 2013). Soft-Tissue Injuries Other Than Lacerations. Village Medical Manual: A Layman’s Guide to Health Care in Developing Countries, 2 Volumes (6th Ed.). (pp. 70-75). William Carey Library
17. Watters, D. A. K., et al. (September 3, 1991). Burns. Care of Critically Ill Patient in the Tropics and Sub-tropics. (pp. 212 – 232). Macmillan Education.























(File -> Save Page As… -> /surv-stuff/med/trauma/burns) Thanks IvyMike.
Question: On the trip to Parkland, does the fluid volume change based on how the fluid is administered? Thinking of a griddown situation where it might be necessary to use a combination of routes of administration due to lack of supplies. PO, SC, IV, or rectally – just add them up toward the goal? Or would the route change the amount of fluid, or the time it should be delivered in?
LikeLike
Great question Ralph. The thing that we’re looking for in adults is urine out of .5mL/kg/hr, which is 30-50mL/hr and 1ml/kg/hr in peds. The urine output lets us know that the patient is getting enough fluid to keep his tissues perfused. Whatever route you are using, just make sure you are getting good urine output.
Keep listening to lung sounds and watch for pulmonary edema. Back off fluid if it starts getting into the lungs.
On circumferential burns on extremities, keep checking distal pulses, because the patient is going to continue to swell over the 24 hours from the time of burn. Hopefully you’ll have an experienced practitioner that can make the call on escharotomies if needed.
One thing I forgot to mention in the big piece is that the calculations for fluid resuscitation are based on fluid over 24 hours from the time of the burn, not when first medical contact is made. So in a remote location, a patient that gets first medical contact 8 hours after his burn means you have 16 hours to get 24 hours worth of fluid in him. That will heighten the risk of the conditions above, but you have to do what you have to do.
Hope this answers the question.
LikeLike
That answered it, thanks. Think I may have subconsciously chose to ignore the “A Foley catheter will be inserted…” part of the article. Not an item I currently have in stock, nor one I really want to learn to insert.
LikeLike
Reblogged this on South Carolina, Free! and commented:
Medicine is important. Take care of yourself, then your family, then your neighbors, then your community.
LikeLike
Very impressive write-up!
The part about flying through the nuclear tests was shocking to me – as a former AF pilot we never heard that story. It seems the key screw up was flying under overcast (oopsie!). Glad it was him and not me.
At any rate, while the books say mild symptoms of ARS may happen at 0.3 Gy, that just means that if you tell someone they have been exposed to ionizing radiation they may get nauseous. The chances of actual signs at that low an exposure are … meh.
WRT honey (which I advocate as a pretty good wound dressing in the right circumstances) I feel that it should probably be processed and at least pasturized, rather than raw. Raw honey (straight from the hive) has G-D knows what in it and putting something contaminated on a wound (burn or not) seems wrong to me.
LikeLike
Great point on the honey Doc. Thanks. Agree. Same on ARS. Former life had me dancing around nuke plants with regularity, and I loved to give my speech to people about the radioactivity in their bananas. Something is gonna kill us all. Act accordingly.
Glad Generals LeMay, Ripper, or Turgidson didn’t have you flying through mushroom clouds. Sounds like a sh*t billet.
LikeLike
Flying F4’s, prepping to turn the Fulda Gap into a glass parking lot, what could be better (except Med School)?
LikeLike
@flighterdoc:
That’s badass.
LikeLike
That is some seriously cool chit flighterdoc. Sorry for my part if we got off on the wrong foot in an earlier post.
LikeLike
No problems…
LikeLike
At ground level one of my basic digital geiger counters runs about 14 -18 CPM. In the airport x ray it recorded 320 CPM for a few moments.
It ran 360 CPM for the duration of the flight.
Was a fun experiment.
Over 10 yrs ago I provided med oversight for the guys guarding the tuwaitha reactor in Bagdad for a short time.
So aparently a stolen cooling rod made for a great bread roller in the local bakery until it was recovered…..
As for unfiltered honey off my hives it has wax and bee bits in it. much of this is filtered out in the basic processing I do.
There is a ban on Chinese Honey imports to the US so its heated and filtered to remove polen so its source cannot be identified and then sold to India for resale to the USA. The point is that its heavily filtered but has been heated. Still if any enzymes are still active you will note that nothing will grow in it. If the enzymes have been cooked out the osmotic pressure of the sugars will still crenate most bacteria present hence it does not spoil. BTW This pressure also pulls edema out of a wound like a vac dressing resulting in better blood flow to the wound base.
Bees are very clean. Bee wax is inert and used as “bone wax” and left implanted surgically its so inert.
I would sugest that even the crudest honey scooped from a wild hive is much cleaner than most open wounds that are hospitable to pathogens that are found on the skin normally.
Thats just my take on it, I have been wrong before. If you are worried heat it to 70 deg C for 5 min and call it good.
LikeLike
One might also profit from an investigation into the early 20 centur/late 19th century use of tanic acid (STRONG tea or tea from acorns or other sources of tanic acid).
Effectively, one is tanning the burn skin, and there had been improvements in healing results.
One source for grid down tx for burns refers to use as a cooler for the burned skin..http://www.doomandbloom.net/natural-burn-treatment/
(These folks are pretty solid)
Interesting additional reading including complementarhy treatment options:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3495394/
Additional reading on tannic acid tx in burns:
https://www.google.com/webhp?sourceid=chrome-instant&ion=1&espv=2&ie=UTF-8#q=Use+of+tannic+acid+in+burn+treatment
LikeLike
Since honey can support C. botulinum, (which is why we don’t give it to infants) I don’t think pasteurizing it is a bad thing…
LikeLike
Quick reply between patients:
Botulism is an anaerobe that can be found in Honey at times. It has the potential to cause infection in a deep puncture type wound but not in a shallow wound. I read a study on the use of non irradiated Honey in wounds and they could not find a single case of botulism infection in burns or ulcers. Sorry I dont remember how many hundreds of wounds were treated. I think this is the right study,
The therapeutic use of honey.
Bell SG
Neonatal Netw. 2007 Jul-Aug; 26(4):247-51.
Normally medical honey is irradiated with a gamma source as a precaution.
Heating to 120 deg C for 10 min is needed to be rid of botulism. Unfortunately this negates some (but not all) of the positive effects of the Honey in the process.
Main pathogens in Burns include …. here I will cut and paste from my hard drive from I forgot where originally sorry.
——————————————————-
The pathogens that infect the wound are primarily gram-positive bacteria such as methicillin-resistant Staphylococcus aureus (MRSA) and gram-negative bacteria such as Acinetobacter baumannii-calcoaceticus complex, Pseudomonas aeruginosa, and Klebsiella species. These latter pathogens are notable for their increasing resistance to a broad array of different antimicrobial agents.[3, 4]
Burn wounds are also commonly infected with fungal pathogens. These infections are frequent after the use of broad-spectrum antibiotics. Candida albicans is the most common fungal infection[5] ; nonetheless, a trend towards nosocomially acquired, intrinsically resistant fungal infections (eg, Candida krusei) has been reported.[6]
——————————————————–
All of these main pathogens are sensitive to treatment with Honey.
Molan, P.C. (2001). Potential of honey in the treatment of wounds and burns. Am J Cin Dermatol 2 (1), 13 – 19
Hope this helps.
On coloidal silver it may slow wound healing
Atiyeh, B.S., Costagliola, M., Hayek, S.H., Dibo, S.A. (2007). Effect of silver on burn wound infection control and healing: Review of the literature. Burns 33, 139 – 148.
LikeLike
Whoo-hoo! A serious lurker on this site, you have hit on my specialty – health physics. An article I wrote on how to protect oneself in the event of a dirty bomb, which provides response info in a practical (down grid?) way, is at http://atomicinsights.com/dirty-bomb-advice-from-larry-grimm/ .
An interesting story related to how different tissues are affected differently by radiation:
Oregon prisoners volunteered in the ’60s to undergo gonadal radiation studies. They were given X-ray doses up to sterilization levels (600 Rads/Rems for us old rad guys or 6 Sv for the friggin’ Frenchy system lovers). Spermatogenesis has about a couple dozen (27 is what I think) developmental stages and one stage is extremely resistant to radiation damage. All of the subjects had full spermatogenesis within two years, with the lower dosed subjects mostly recovering within six months. DNA analysis was not yet developed, so no info is available whether or not there was permanent DNA damage being propagated.
Radiation damage is all about the dose and tissue type. If the tissue rapidly divides and is undifferentiated, it is much more susceptible to radiation damage. This is why mucosal tissue damage (vomiting) such as in the alimentary canal, is the first indication of high dose. Slowly dividing and differentiated tissue is less susceptible to radiation damage – such as nerve tissue like the brain. You noted these factors but I like to stress it.
To all here, note that if you are dealing with a radioactive material, it is a chemical first and foremost, so think about how to manage the chemical first and you can mitigate a lot of problems of radiation exposure, e.g. if it is a chemical dust, wear a mask or if the chemical is on the skin, just wash it off (light, frequent washings, do not use scrub brushes). I’ve had radioactive chemicals on my skin more times than I care to count and not once did I see a physiological response or damage.
Alpha emitters pose zero risk from an external (skin) exposure, but are a major problem if an alpha emitting radioactive chemical is ingested. Externally (skin) received beta emissions at worst can only cause second degree burns. As long as the chemical is not transferable, I’ll hold an alpha emitter in my bare hands.
The fallout from a nuclear bomb blast contains mostly beta emitters. Islanders who got fallout during nuke tests would put the beta emitting ash on their skin. Burns resulted, but all were healed by six months. Beta emitters that are ingested have about the same damage ability as gamma emitters which is about 20 times less than ingested alpha emitters. The highest energy beta emission can only penetrate about 7 – 9 mm (for Frenchy lovers, 3/8″ for us old farts) into skin so no external beta emissions can reach critical organs.
It makes no difference, other than duration of exposure, whether a gamma emission dose is received from internally deposited chemicals or whether it is external.
You did not mention neutron exposure. There are very few neutron emitters and there are only a couple exposure routes for which one has a low probability of running into, e.g. nuke bomb blast, moisture gauges, neutron therapy, and space travel . Ingestion of a neutron emitting chemical is highly unlikely, but external exposure is possible for the above scenarios.
I can provide a ton of info on radiation exposure treatment but one comment to remember: if you think you have been exposed to high levels of radiation, but you are not vomiting, there is no major hurry to get treatment. One humorous but true comment: if you ingest your tritium gun sight, drink a lot of beer – tritium is rapidly flushed from the body via a high fluid intake.
LikeLiked by 1 person
@aGrimm: This is excellent. You are inspiring another post.
LikeLike
Very nice writeup as well, thanks!
LikeLike
Re the myth of of iodine as a “treatment” for radioactive iodine.
First of all, the use of iodine as a “treatment” only works if the radioactive material is an iodine such as I-131 and I-125. It has no effect for any other radioactive material whatsoever. Zero. None. Nada.
Secondly, the use of iodine is quite good as a prophylactic to prevent thyroidal uptake of radioactive iodine, but poor as a treatment once the radioactive iodine has been taken up by the thyroid.
If you ingest/absorb iodine, radioactive or not, about 50% is taken up by the thyroid in the first 6 hours and about 75% at 24 hours. Once taken into the thyroid, the iodine remains locked in until it is used in the T3/T4 processes. Essentially the thyroid is a bank that can hold a lot of iodine, but it can become full and not take in anymore iodine. Excess iodine is egested via sweat, feces and urine. This is where the idea of using iodine tablets comes into play – flood the body and thyroid with so much normal iodine that the thyroid becomes full. Subsequent ingestion of radioactive iodine becomes diluted in the large iodine pool. Though some radioactive iodine will likely be taken up by the thyroid, far less will be taken up. The bulk of the excess free iodine is excreted fairly rapidly.
Your body will take up any elemental iodine that comes its way. It will be taken in via respiration, ingestion and even absorption through the skin. Skin absorption happened to me – through two pairs of gloves nonetheless – when I worked for a company that manufactured I-123 .
The prevention of thyroidal radioactive iodine uptake is time sensitive. So if you are downwind of a power plant explosion, you need to take the iodine tablets immediately, but remember that it will take awhile for the tablets to flood the thyroid. You will likely still get a tiny amount of radioactive iodine in your thyroid if your exposure is concurrent or within a few hours of taking the tablets. It is best to take the iodine 24 hours before the exposure, but you need to be prescient or forewarned that you are going to get the exposure. One problem with iodine tablets: a small percentage of the population will react poorly to large quantities of free iodine in their body. It is a very small risk, but one to consider.
If the radioactive iodine is airborne, the better prophylactics are a charcoal filtered mask and disposable clothing which also work well for all the other radionuclides except a couple of the gases.
If the thyroid has taken up radioactive iodine, the main treatment is Lugol’s solution which contains a large quantity of iodine. This has limited success because it principally acts by molecular exchange, in other words a non-radioactive iodine molecule has to replace a radioactive one in the thyroid and this doesn’t happen easily.
Personally, I don’t keep a stock of iodine tablets unless I plan to go hiking where the water could contain nasty stuff. The tablets have a shelf life and what are the odds of an iodine exposure when the nearest nuclear power plant is hundreds of miles away? However, if Iran gets the bomb…
LikeLike
This is exceptionally valuable, and I really appreciate you posting it. One thing it drives me toward thinking is “don’t let burns happen in the first place!”
What are your thoughts on using burn pads/sheets as a first aid measure?
(Ones like these: http://www.galls.com/water-jel-sterile-burn-dressing-8-inch-x-18-inch#.VUwKN_lVhBc )
LikeLike
In the pre-hospital setting, I think they are fine, especially for superficial burns and the less severe partial thickness burns. The gel will help cool the burn and the dressing will keep air from flowing over the burned skin, which can help with pain. Know that whatever dressings you put on are going to come off at the burn center as they get cranking on managing the wounds and doing fluid resuscitation. Glad you found the post useful.
LikeLike
Gel dressings are heavy, expensive, the wrong size for the wound, bulky if any bigger than 4×8, and yet absolutely nothing works better for putting out the rare wound of burning WP.
LikeLike
Well I just learned something new today. Cool.
LikeLike
Hey guys, bump, due to the fireball at the concert in Taiwan, lots of severe burns, lots of pictures.
http://www.dailymail.co.uk/news/article-3142946/Female-Taiwan-pool-party-fireball-victim-20-die-burns-explosion-left-500-people-seriously-injured.html
The fireball was apparently caused when a large quantity of powder, cornstarch with coloring agents, was sprayed into the air over the crowd.
I can’t imagine that they have enough burn centers in Taiwan to care for these kids. I think we would be hard pressed.
nick
LikeLike