Well, now that we have established you can improvise a video laryngoscope (VL) for less than $50, we move to the process of ventilating your patient.
The fashionable airway has a few must-have accessories: 1) a ventilator, that moves air in and out, 2) an oxygen source, 3) monitoring capability for O2 and CO2, 4) inline suction sources to clear the airway, 5) a means to secure the endotracheal tube in place, and finally 6) some form of sedation so that your patient doesn’t go crazy and wind up with PTSD.
And of course you have to be able to do all this on the cheap. Well, I will at least. Despite my doctor level income, I’m still a cheap bastard, much to my wife’s dismay.
Ventilators:
I’m not going to go over, in this or maybe any other post, all the ins and outs of managing a vent. It’s not trivial. You really do need someone with grid-up, formal training to run one. So make friends with your friendly neighborhood respiratory therapist, or any of a host of different types of physicians (Internal medicine, surgery, anesthesia, Pulmonary/Critical care).
Vents are fairly complex machines. They are spendy: the one at the top of this post is about $10,000, used. They are resource hogs: most modern vents require not just electricity, but compressed air and compressed oxygen. The vent uses the pressure of the gasses as the source for the pressure used to cycle the air in and out of your patient. And while you may have your solar cells banging out the watts, a constant source of 50 psi gasses are harder to come by. Welders, perhaps, may have a line on such things. But I digress.
There is a category of vents that do not require compressed gasses to work, as they have built-in compressors. These are called “portable vents” and are in general used in transporting the patient from one hospital to another in an ambulance or helicopter, transporting an ICU patient down to get a CT, and are also used at home by folks with neuromuscular diseases like Steven Hawking (although apparently he doesn’t need one yet. Astonishing). They also run on battery power. So if you can lay hands on, say, a bank of solar powered batteries, you might just be in business.
For our purposes, we will focus on just one type of vent: (but please note there are other, more modern vents out there) the Eagle Uni-vent 754. It looks like this:
The user manual is found here. Please ignore the oh-so-cheesy garbage in the intro: “And where the eagle is known for its keen sight -this Eagle sees a future that no other portable ventilator has ever seen.” Oh brother.
It can run off compressed gasses if you need it to, but can also run on its own internal compressor. On ebay these run between $750 (as is, untested) up to $5000 (user refurbished with a limited guarantee).
or…
You could go to the website www.govliquidation.com, and there search for “portable ventilator“. I have it on reliable authority (pa4ortho) that the vents go for about $400, but as always, YMMV. And hey, you paid tax dollars for the military to buy these things, might as well get some of it back. One more thing, there is an FDA form that you must complete on the GovLiquidation web site that affirms that you are; a) a licensed medical practitioner, or b) medical equipment reseller that only sells to licensed medical practitioners. After all, this is a purchase from the government.
It will run off regular air, and you can use low-pressure O2 should your patient need some extra oxygen. The way to do this is to close off your high pressure oxygen port, and blow your extra oxygen source (covered below) directly into the ambient air intake.
But what if I don’t have that, doc? What if I’ve only got $50 lying around and I need a vent?
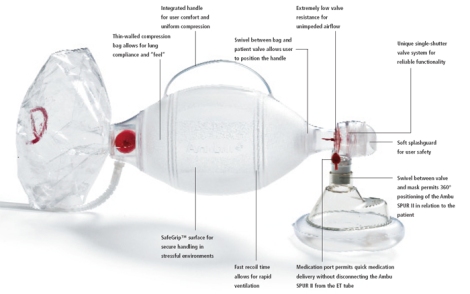
Well, then, drop your coin on an ambu bag. Get the one with the PEEP valve, it’s worth the extra money. The adaptor that holds the face mask portion, is also the right size to attach to an endotracheal tube.
To run this you will need the oldest vent known: you. That’s right, you sit bedside and give your buddy a breath every 5 seconds by squeezing the bag with one hand. It’s very resource-intensive, but it’s what they did for the polio epidemic, as there were only about 1000 iron lungs (the gold standard at the time) but around 9,000 patients.
“Intensive use of positive-pressure mechanical ventilation gained momentum during the polio epidemic in Scandinavia and the United States in the early 1950s. In Copenhagen, the patient with polio and respiratory paralysis who was supported by manually forcing 50% oxygen through a tracheostomy had a reduced mortality rate. However, this heroic intervention required the continuous activity of 1400 medical students recruited from the universities. The overwhelming manpower needed, coupled with a decrease in mortality rate from 80% to 25%, led to the adaptation of the positive-pressure machines used in the operating room for use in the ICU.“–Medscape
As you sit by your buddy, you will note several things. It’s harder to give a breath when he is trying to exhale. And it will be very difficult for you to precisely regulate how big of a breath, and how frequently you give him one. “Bagging” someone is a temporary thing, as you will quickly discover. Not that it doesn’t happen out in RealityLand, but it is typically limited to paramedics bagging someone on the way in from the crash site.
IvyMike adds: Speaking of ventilation with an ambu bag, a couple of basic pointers. Adrenaline is an amazing thing, and when you, the rescuer are full of it, your count is going to be fast, so you have a good probability of bagging too fast. An intubated adult patient should be getting 8-10 breaths per minute. A non-intubated adult patient should be getting 12-20 per minute, with the emphasis on 12, not 20. Let the ETCO2 [a measure of the clearance of CO2, described below] and the patient’s condition guide your ventilations. Also remember that people don’t breathe in violently, so don’t squeeze the hell out of the ambu bag. Nice and easy, full one-second or longer inhalation phase. You don’t need to empty the entire contents of the bag into the patient’s lungs with each breath. Average tidal volume for a patient is 500cc, and the ambu bag has the ability to give 1000cc to 2000cc, so don’t blow the patient’s lungs up. Get good chest rise and fall, and watch the ETCO2. Fire up some Bob Marley and get Mellow. Very mellow.
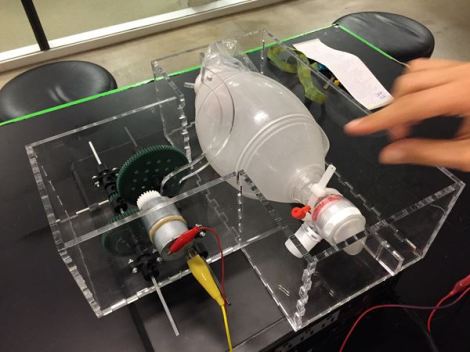
So what if you decided you would like to make a vent-like device on the cheap? One that uses your little ambu bag and a computer-driven device that could squeeze the bag, instead of you? You’d have to control the size of the breath you give (tidal volume) how quickly it is given (flow rate), how often you give a breath (respiratory rate), the amount of oxygen (Fraction of inspired oxygen, FiO2), and the positive end-expiratory pressure (PEEP). But you could probably put something together. Something like, say, this.
This nifty little bit of kit is put together as a design challenge for a group of engineering students at Rice University in Houston. Looks like they used plexiglass and legos to make something that would actually work. They note on the website they have gone through the calibration steps, and they are now in a more advanced prototype stage. They did use their laptops to control it, and you will note they used rotary motors. However, with the advent of all the recent Arduino tech, this becomes a basic project for a competent Maker, computing and all. All of the components can be obtained at your local Home Depot and Radio Shack. Interesting, no?
It would lack some of the bells and whistles (and alarms) of a real vent, or even a portable vent. Currently vents use a small continuous flow of air to detect pressure changes and also to detect when a patient is trying to take a breath. Just like when you are bagging a patient, you want to work with his respiratory cycle, not against it. The above mock-up has no ability to detect patient-initiated breaths as the ambu bag has a couple of 1 way valves to prevent backwards flow of exhaled air. You would probably need to put a sensor around the chest so that you would be able to determine when a patient was taking a breath. That way you will be able to work with his breathing pattern instead of against it. This, by the way, already exists as off-the-shelf technology, so there’s not much “creation” needed. You’d have to watch your buddy closely, so that nothing disconnected and nothing went wrong, clinically. But you’d be able to take a piss without killing him. And you could probably monitor several folks at once, exchanging manpower needs for electrical needs in your fancy grid-down hospital.
Oxygen Source:
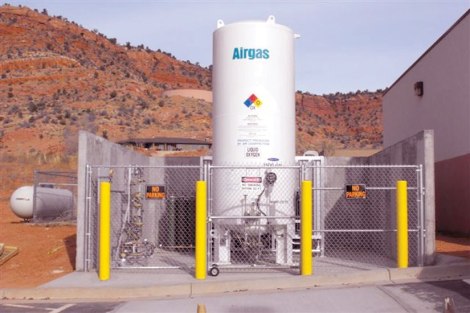
Grid up, we use a combination of liquid oxygen and oxygen tanks, as seen above. These are usually massive, permanant structures that can feed 50 psi oxygen to every room in a 450 bed hospital for 96 hours. You’ll not have that.
There are a variety of oxygen concentrators available that remove oxygen from the atmosphere and concentrate it into useful levels of oxygen. They vary from industrial sized units that can provide the 50 psi gasses that true vents like (pa4ortho indicated that this is what they used in the military’s mobile hospitals), down to home-portable units that individual patients use for their COPD (see here, but dozens of examples available), and some hybrid units in between. Increased costs gets you increased capability, but also remember that you have to exchange electricity for oxygen in this setting, and the larger ones are real energy hogs. Consider not just the up front cost but also your potential grid-down electrical sources carefully, as there is no such thing as a manually powered oxygen concentrator.
Monitoring Capability:
A very brief primer on gas exchange: Your body combines glucose with oxygen in order to efficiently create energy. All of you have heard of aerobic metabolism, which uses oxygen, vs anaerobic metabolism, which doesn’t. You get around 15x more energy per unit of glucose when you use oxygen.
The waste product from metabolism is carbon dioxide. The harder you work, the more it produces. Via a set of chemical interactions I won’t go into here, carbon dioxide also creates a very efficient buffer system that allows you to control your internal acid/base balance.
Getting oxygen in, and carbon dioxide out, obey two different sets of rules. From a ventilator perspective, your oxygen levels are determined by the fraction of inspired oxygen in the air (FiO2) and the average amount of pressure in your lungs that hold them open (determined by the Positive End Expiratory Pressure, or PEEP). In general, this raises the amount of oxygen in your lungs. That oxygen obeys one of the fundamental rules of chemistry, which is: things naturally flow from a high concentration to a low concentration. High FiO2 and PEEP form a high concentration, and your blood is quite a bit lower, so the oxygen flows into your blood and is picked up by hemoglobin. The hemoglobin is required, as the liquid portion of your blood has almost no ability to carry oxygen.
Carbon dioxide, on the other hand, dissolves very well in the liquid portion of the blood. The muscles and other tissues form a high concentration, and your lungs have a very low concentration. (Despite the yammerings of the global warming crowd, in this context the concentration of CO2 in room air is functionally zero.) There is no need for hemoglobin, although it does help, and removal of CO2 depends on how much air you can get in and out per minute. That’s calculated as the size of the breath you take (tidal volume) x the number of breaths per minute (frequency or respiratory rate).
Grid up, we use a combination of pulse oximetry to measure oxygen, and arterial blood gases (ABGs) that can measure both O2 and CO2, although ABGs are nowadays used mostly to check CO2. You can use capnography (described below) but in most medical ICUs that hasn’t caught on yet. Pulse oximetry and capnography are relatively straightforward to use in a grid-down situation, although the latter may be prohibitively expensive. ABGs, not so straightforward, and also expensive.
Easy thing first. Get a pulse ox on his finger. A pulse ox monitor uses reflectance of various wavelengths of light on oxygenated and deoxygenated hemoglobin to tell you what percentage of the hemoglobin is loaded with oxygen. For the purposes of simplification, the number is pass/fail: 90% or above is a pass, below is fail. They are available cheap on Amazon, with AAA batteries that you can replace with rechargeables from your solar cell panels.
There are limitations with this tech, that mostly revolve around artifacts from patient movement or poor perfusion. Get one that shows the waveform (the wavy blue line on the example above), it allows you to distinguish artifact from real data. And watch this excellent video from the NEJM describing the tech in more detail:
The challenge is determining if your patient is clearing CO2. Progressive buildup of CO2 makes your body very acidic, will make you sleepy, and eventually cause your entire cardiovascular system to collapse. Of our two very expensive options (and the main limitation is expense), I think capnography is the better grid-down choice.
The next bit is modified from IvyMike’s input:
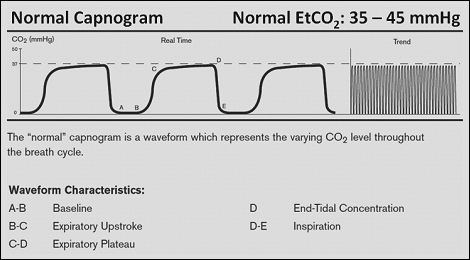
End-tidal CO2 waveform capnography is a Godsend to medical people everywhere. It measures how much CO2 the patient is blowing off via a sensor inline with the ventilator tubing or ambu bag. Either on a ventilator monitor or cardiac monitor, the CO2 will be graphed out as waveform with measurements in millimeters of mercury (mmHg), with a normal adult range being 35-45mmHg. The waveform looks like so:
In addition to being the best way to confirm an ET tube placement, this little guy right here will help you dial in your ventilation. If the ETCO2 drops below 35mmHg, then your patient is blowing off too much CO2 which could mean your minute ventilation (size of breath x number of breaths per minute) is too high. If you are bagging with the Ambu, you are going too fast or squeezing too hard, or both. If it goes above 45mmHg, you might be going too slow or your patient is pretty sick. Never be surprised when you first get an ETCO2 reading and it’s off the charts high. If your patient has been in respiratory distress or failure, he’s probably built up a lot of CO2 in his system, and ventilation is the way to help correct that.
In grid down, good luck getting ETCO2, however. There are portables that retail for a mere $9,000. Grouch notes: I found one here for $1800; a search for “refurbished” yields few options that run less than $1000. The little beauty above–an EMMA II capnograph–runs $1100 or so, but really there’s no excuse for them to be that expensive. I have to believe in our current, disruptive technology environment, some enterprising youngster can create a hack with a sensor and an iPad.
[Update: Dr. Grouch inquired among the enterprising youngster crowd, who feel it is unlikely that the actual production cost of the EMMA II above exceeds $100; the other $1000 is recouping development and startup costs, as well as the glories of capitalism. I asked how one would hack a dirt-cheap version, and said enterprising youngster says: “If you can find the factory in China where it is made, it’s easy…]
[Update to the update: it appears that said enterprising youngster may actually have an interest in disrupting the high cost capnograph industry. It won’t happen for a while, but if it actually does happen you, loyal reader, will know…]
Suction:
This is a bigger deal than you think. Once the endotracheal tube is in place, there is no means for your patient to cough. However, your lungs will still produce mucus, and if you have a pneumonia on top of that, you’ll make even more. If that isn’t pulled out somehow, it will block off your shiny new ETT, as well as all of your patient’s airways, and kill your patient. And I assure you, as a doc that works with this for a living, that’s not theory but practical reality.
Grid up we use the hospital vacuum system, and a special adaptor on the ETT that allows in-line suction. We do this so that the circuit is not broken (that is, the ETT is not disconnected from the vent) because frequently we are relying on the pressure built up in that circuit to help oxygenate the patient. Because it’s medicine, and therefore people go bananas with protocols, this has turned into a big deal, see example here.
You can also simply disconnect the ETT/vent circuit and suction that way. Any relatively firm tube will do. It would need to have an outside diameter at least 1.5 mm less than the inside diameter of your endotracheal tube, be about 40 cm long, and have the ability to hook up to your suction source.
There are many manual or foot powered suction sources, see video below.
Securing the ETT in place:
Obviously you don’t want it to fall out. More commonly, however, your buddy gets agitated (ETTs hurt, and they make you feel like you are constantly gagging yourself) and pulls the thing out himself. When he does so with the balloon still up, he runs the risk of tearing his own vocal cords. This is suboptimal not just from a speaking point of view, but it also messes up his ability to breathe correctly.
Grid up there are a host of possible options, from simple tape up to more complex devices like the one pictured above. The above is the specific device used in my hospital.
pa4ortho recommends the following for grid down or wilderness med approaches:
“One other tip is in securing the ET tube tie a single Prusik knot out of IV tubing on the ET tube. Pull it tight and the IV tube flattens and grips the ET tube. Wrap around the back of the neck and tie on the side. On a mannequin you can lift it off the table by the ET tube without dislodging the tube.”
For those not familiar with the knot, there are a couple of ways to tie it:
Sedation:
Grid up we use IV drips or pushes of narcotics and propofol. As Michael Jackson taught us, the latter is not to be trifled with. Grid down, you will end up using a combination of reassurance, and whatever medications you have available. These might include, but not be limited to, pain pills of any type, sedative pills of any type, alcohol (orally or IV), or ketamine (as a continuous infusion). Avoid the harder drugs like cocaine or meth–while I’ve no moral qualms about using them in an emergency, grid-down situation, they are too short acting and have rapid swings in their effectiveness. Cocaine, for example, would make your intubated buddy really happy for about 30 minutes, then normal for a bit, then in a deep, dark depression for about a hour. Then he gets another hit and cycles through again. Doesn’t sound like the right thing for your patient, and almost guaranteed you’d have to deal with the problem of an addicted patient once he came off the vent.
Conclusion:
So there you have it. A decent jump on many of the things you need in order to make up the respiratory section of your grid down hospital. I’ll take this moment to re-emphasize that you need to have someone around that has had experience running vents before. It’s complex, and lots of things go wrong. I would also re-emphazise the harsh reality that if you don’t have any means of correcting your patient’s respiratory failure, you’ve no business subjecting them to the torture of having a breathing tube rammed down their windpipe.
—————————————————————–
Disclaimer: Neither Doc Grouch, nor the faculty of Hogwarts, have any financial interest in any of the products above. Nor do we have any financial interest, period. Shoot, we aren’t even an Amazon affiliate. We don’t specifically vouch for, endorse, or recommend any particular product. Do your own homework, and caveat emptor.






Waaay above my skill level,although I do have some practice in pulling out tubes by myself-usually not very far,as it seems to set off all kinds of alarms,and bring all kinds of medical staff running. I have found that clamping my teeth down on the tube prevents re-insertion,and generally results in communicating with the Dr. -which is hard to do with tube down your throat-and agreeing to allow tube to be re-inserted if I can’t breathe on my own when they take it out.
Fortunately-I was able to breathe on my own both times that scenario played out-one of the 2 times,I required oxygen,the other,I had enough oxygen in my system within 2-3 minutes.
Back to the subject at hand-anyone with the $$$ ,a building,and the connections in the way of Dr’s,RN’s,respiratory therapists,Nurse practioners,LPN’s,med/surg nurses,etc. should probably invest in medical equipment,and large diesel generators ASAP.
Or start studying the military’s mobile field hospital set -ups,and purchasing what’s needed to duplicate one.
I have a respiratory therapist, and an RN that likes working the ER as neighbors,several houses away-I just planted veggies that they asked about in my garden-and will be delivering plenty of said veggies to both when the crop comes in,along with the hot pepper rings I can each fall that they like.
Never know-might have to depend on them at some point in the future.
LikeLike
Dear Dr. Grouch,
Sir, with all due respect, I admire your verve, attitude, and your obvious love and compassion of life. The information presented is indeed a cliff notes synopsis of many rudimentary aspects of critical care. You are to be commended. Thank you.
That said, the level of expertise, the equipment required, the knowledge, and of course the funds required to come to the levels that you suggest, to name a few, in the times to come, suggests to me that when M&M conference is held, there will be quite of few cases to be reviewed and discussed.
May God in his infinite wisdom look out for us all.
LikeLike
I thank you for the compliment.
I agree in detail with your concerns about the outcomes in a grid-down scenario. It will be ugly, and I have only barely brushed the surface of the required information needed to set up a grid-down ICU.
Which does not exempt me from the moral obligation to try. I recognize, however, that if a grid-down “tribe” does not have someone with extensive grid-up experience in doing these things, I do not think it possible to teach them all they need to know via this blog. Assuming they can put something together at all, mistakes will be made, complications will arise, and people will die. Assuming those acting as medical professionals have the courage to continue forward despite these setbacks, M&M will be integral to their learning process, as you have pointed out.
Again, thanks for your comments.
LikeLike
So kind of you to mention Government Liquidation. We appreciate the shout out! If anyone has questions about bidding or about the FDA form, I would be happy to help.
LikeLike
Thanks for stopping by Robin. I do have a quick question on the FDA form. What constitutes a “licensed medical professional?”
I assume advanced and mid-level providers like; MDs, DOs, PA-Cs, and NPs are included, what about RNs, CRNAs, and paramedics with current certifications? Also, basic providers like EMT-Bs, CNAs, etc?
Thanks for any help, your site is a great place to burn up excess money!
LikeLike
Hi IvyMikeCafe! Yes, anyone who is a licensed medical practitioner and/or someone who regularly and lawfully engages in the manufacture or refurbishing of medical and dental equipment. As for stopping by, I was really excited to run across this article. It’s great to be included in an informative post like this. Government Liquidation fills a unique niche within the medical community, and we’re doing our best to assist those who assist others.
LikeLike
Pingback: Hogwarts: “Any of course with that shiny new airway, you’re going to need some accessories…” | Western Rifle Shooters Association·
Your mention of an ambulance bag and mechanized adaptations of it beat out my lingering question of the viability of considering negative pressure respiration. A long time ago an emt aquaintance on a forum discussed iron lungs as a cheap alternative to the expensive respirators currently used which would be in short supply during something like a flu epidemic.
Any rigid tube could be improvised into a low pressure single stage compressor, and with a stepper or servo for power, volume given is easy. I’m sure if you looked you’d find a dozen vents a hundred times better than an ambulance bag and a motor for a similar price.
As a manufacturing major, I can asure you that machine vision has come a long long way. Good stuff is expensive, but if you can find a reliable surface observable phenomenon that will correlate a chemical level, all you need is a cheap Webcam and the right light source. The rest is programming and testing and verification.
LikeLike
What about using a bipap machine for airway support? This is more common in homes because people have sleep apnea. (Just find an very overweight person with good insurance and you might score one.)
Since bipaps are designed for home use it might be a better option. Isn’t bipap a type of vent- a non invasive one?
If there is no sedation in grid down scenario we should all be DNI.
LikeLike
Bipaps are good but have their limitations, if the goal is to use it to replace a true vent, hooked onto an ETT. By itself, it is a very handy tool, and we use it all the time in the ICU. They are not as common on the outpatient side as CPAP machines, which is what most folks use for sleep apnea. However, they can help some very sick patients breathe, and get them over the hump.
A bipap machine is not quite as good as a vent, but in a grid down scenario that may be a feature, not a bug, if a ruthless one. If your breathing is so bad that you fail bipap in a grid down scenario, the chances you are going to make it at all, are quite low. It sounds cruel, but in a limited resource environment, you can’t spend resources you don’t have on people that aren’t going to survive regardless of your efforts.
THere are many folks who tolerate the vent with very minimal or no sedation. I would only make someone DNI if I had no effective treatment.
…but I’d want some sedation, let’s be honest here…
LikeLike
Thanks.
I am an RN at a level 1 trauma center. However I usually only see chronically I’ll people. I work on a progressive care floor where rescue bipap means change in level of care.
I like your website. Thanks for putting the time in to make it work.
LikeLike
Glad to be of help!
LikeLike
Ok so I have not tried it yet but for an air supply for a non eagle vent heres a thought….
You can get a portable dental (oil free) air compressor unit from ebay for around $500.
Now you have a nice dental tool as well as an oil free source of compressed air. Just check air pressure and volume on the unit you want to get. It needs to have a resovoir tank and be oversized to run continuously.
FYI 1 Kg/cm2 = 14.2 Psi so anything up to or over 6Kg of pressure should work.
No an oily air compressor in the garage will not help! It will coat the lungs and cause pulmonary edema.
I have a few bipap machines for respiratory management of viral or bacterial pnumonia. There are several good articles I have read on this. Its a whole new post topic in itself.
boat pumps or 60 cc syringes can be configured to provide suction. I have some foot powered and 12v set ups and a big 110v suction unit.
Suction is the most under apreciated task to the novice at this. If you dont think suck you suck….. Tons of untested guys are running around downrange with the idea and kit to get an advance airway
LikeLike
Inhalation of oil of any type leads to something called “lipoid pneumonia”, see here for example. It’s not good, and devilishly hard to treat.
LikeLike
I have a rude modification to the ABCDE assessment pneumonic.
“A” is always “assuck” in my head, to always remind me to have portable suction on hand. It is low-class, rude, and effective for me.
LikeLike
Ivy Mike….did you get any information back from Government Liquidation on what constituted a licensed professional? I think resellers can also buy from them but am not sure what that requires either. (sales tax # and tax id # ?) I have looked at their med equipment over the last year or so but have not tried to bid on any. I do have a Doctor, Nurse, and Vet in the family tree and would like to stash some supplies.
LikeLike
Indy, here’s what I have found so far.
1) The FDA form on govliquidation requires you to select one of the following when you order:
A I certify that I am a licensed medical practitioner and/or other person regularly and lawfully engaged in the manufacture and/or refurbishing of medical & dental equipment. I also certify that prior to sale of use of such equipment I will take necessary steps to assure that such equipment is not adulterated or misbranded within the meaning of those terms in the Federal Food, Drug and Cosmetic Act. (21 U.S.C.311, et seq.)
B Recognizing that Federal law places stringent restrictions on adulterated or misbranded medical devices (2) U.S.C.311, et seq.) I certify that I will sell or otherwise proffer the medical devices purchased only to licensed medical practitioners as described in “A” above. I will not use those items for their original or usual intended use of for any other medical use.
2) A hard and fast definition at a federal level has been a bit of a wild goose chase through multiple agency web sites, US code, and US CFR searches. The morass of bureaucracy yields lots of definitions for “licensed medical practitioners” that are tied to specific areas within the Federal Food, Drug, and Cosmetics Act, (Title 21 USC) and these tend to mean advanced to mid-level providers, which are MDs, DOs, PAs, and NPs respectively. There are definitions for “licensed and certified health care practitioners” as well (Title 42 USC), and those are more broadly defined all the way to social workers. In both cases, the federal law points to the practitioner being licensed / certified to practice in his/her state by a state licensing / credentialing body, so the key is to know what is licensed / certified in your state. Know that a license tends to be more rigorous to attain than a certification, so there’s that.
Since govliquidation is citing Title 21, I’d bet money on the higher-level providers.
In that case, it’s great to have friends in higher-level places.
We also need a much, much, much, smaller government. The amount of micromanagement I read through is starting to make the Soviet Union sound efficient. Ugh.
LikeLike
Hi IvyMikeCafe and indyjonesouthere – I believe my response was posted above, but since there are more inquiries, I’ll try to expound. The FDA form that we’re required to collect looks imposing but is actually very simple. You do not have to be a licensed professional to purchase medical equipment from us. If you’re not a licensed professional, select option B. It’s my understanding that the purpose of the form is to cover the gov’t for liability in the event that someone buys a dental chair, for example, and assumes that suddenly makes them a dentist. Non-practicing individuals buy from Government Liquidation and donate those medical devices to other countries where they are put to use by doctors and nurses in the field. We’re actually moved more than we can say when we hear about folks donating surplus items in this way. That’s why I mentioned that we have a unique place in the industry. If you’d like to see what others have done with items they purchased from us, here’s a link to our YouTube channel: http://bit.ly/OurBuyersAreTheBest
LikeLike
@surplusrobyn – You rock. Thank you for the clarification. Great YouTube channel. Nice to see the gear getting repurposed for good causes. Again, thank you.
LikeLike
My pleasure!
LikeLike
Doc Grouch, Thanks for the peek into my world. I am an Respiratory Therapist (and group med officer). In a total grid down scenario, I cannot envision successfully using respiratory support for more than a few hours. That said, we are persistent in not giving up on our loved ones and team members. I just pray we never get that far down.
Sput.
LikeLike
Ref the cost of the capnograph at 1100 FRN’s, remember that they have to put a per device contribution to the self funded malpractice insurance liability account. It’s like Plano Tackle boxes. The extra 100 FRN’s they charge to put 4 Star of Life stickers in with the box is purely liability. Friend pulls em off the line down the road from here…The Star of Lifes add 100 to the cost..
“First we kill all the lawyers”
LikeLike