Today we’ll discuss shock. In a grid-down scenario, where there is no Facebook, Starbucks, running water, EMS service, trauma hospital, or anything else we’ve become accustomed to in our very wonderful world, a lot of this will be moot without a backup plan in place.
There are several types of shock, and we will cover the ones that are most likely to manifest in a grid-down world, where trauma and infectious diseases like cholera and dysentery can run rampant due to breakdowns in sanitation and hygiene.
Basic physiology
Let’s look at how you are supposed to work on any given day; when the sun is shining, your wife or husband loves you, and the dog obeys your commands. I am going to try and keep this BASIC, BASIC, BASIC, so any med guys feel free to chime in with comments / additions. I’ll probably leave some stuff out in the interest of brevity and because we’re talking field, grid-down medicine here and not ER / OR / radiology lab medicine.
When things are in good order, you are considered to be in homeostasis, which has all of your major organ systems, nervous system, circulatory system, your metabolism, your electrolytes, etc., all in good working order.
Everything in your body is being perfused properly. Perfusion is the supplying of oxygen and nutrients to the body tissues as a result of the constant passage of blood through the capillaries[i].
The capillaries are the smallest blood vessels in your body and are the ones responsible for getting fresh, oxygenated blood to the organ system cells and also removing any cellular waste products and CO2 from the same cells.
Perfusion enables cellular respiration, which in a very basic form, is the burning of glucose (sugar) and exchange of O2 to create energy, with CO2 and waste products being removed from the cell. All of your cells in your body do this to varying degrees. It is known as aerobic metabolism and it means that oxygen is helping to produce large amounts of energy at the cellular level. Anaerobic metabolism has the cell creating energy without oxygen. It creates much less energy than aerobic metabolism, and more importantly, it creates more waste products than aerobic metabolism.

An animation of a typical human red blood cell cycle in the circulatory system. This animation occurs at real time (20 seconds of cycle) and shows the red blood cell deform as it enters capillaries, as well as changing color as it alternates in states of oxygenation along the circulatory system. Source: https://upload.wikimedia.org/wikipedia/commons/7/75/Erytrocyte_deoxy_to_oxy_v0.7.gif
The capillaries pick up the CO2 and waste products, and they flow into the venous system, where ultimately the lungs, liver, and kidneys filter out the bad stuff and blow off CO2.
The lower airway and lungs in gross form, are broken down from largest to smallest airways as follows:
Trachea, right and left mainstem bronchi, lobar bronchi, segmental bronchi, bronchioles, and alveoli.
The airway. Source: https://en.wikipedia.org/wiki/File:Illu_conducting_passages.svg

Bronchiole leading into the alveoli. This is where the gas exchange occurs.
Source: https://en.wikipedia.org/wiki/File:Bronchial_anatomy.jpg
The alveoli are tiny airbags that are the termination point of the lower airway. They are covered in a liquid called surfactant, which helps keep them keep their shape. If surfactant is missing, the alveoli can collapse and bad things will start to happen.
Gas exchange happens in the lungs at the alveoli and capillary beds. The O2 passes through the alveoli into the capillary and thus into the circulatory system, and the CO2 passes from the capillary over into the alveoli where it is expelled through ventilation. Ventilation is the mechanical operation of the lungs and the movement of air into and out of the lungs. Ventilation and gas exchange are related, but they are NOT the same thing. You can have ventilation without gas exchange, which we will cover later.
In order to remain in homeostasis, the body must have adequate ventilation, perfusion, and respiration. The most critical organ systems to keep alive are as follows:
- Brain and central nervous system
- Heart
- Lungs
- Kidneys
- Liver
If one of these systems craps out on you because a breakdown in perfusion, you are having a very bad day.
Shock and the pathophysiology of shock
Shock is also called hypoperfusion, with “hypo” meaning “under” in Greek. If you are in shock, you are not being adequately perfused. There is not enough oxygenated blood circulating throughout your body to keep everything perfused and keep an aerobic metabolism going.
Hypovolemic shock
We’re going to start with hypovolemic shock, which in a grid-down, trauma-prone, life stinks scenario, is the most likely shock you’ll be dealing with because of the kinds of injuries that happen in said scenario. Hypovolemia can also be caused by severe diarrhea, vomiting, sweating, fluid shift, and urination caused by pathogens, medications, toxins, burns, fevers, or other disorders.
Imagine that all of your blood vessels are one giant container full of fluid, your heart is a hydraulic pump to keep the fluid moving, your lungs are your intake and exhaust manifolds, your kidneys, liver, and spleen are various oil filters, and your brain and nerves are your battery and electrical system.
Your container, if you will. Note the positions of the radial, brachial, femoral, and carotid arteries. These are your primary pulse points in a rapid trauma assessment.
Source: https://en.wikipedia.org/wiki/File:Circulatory_System_en.svg
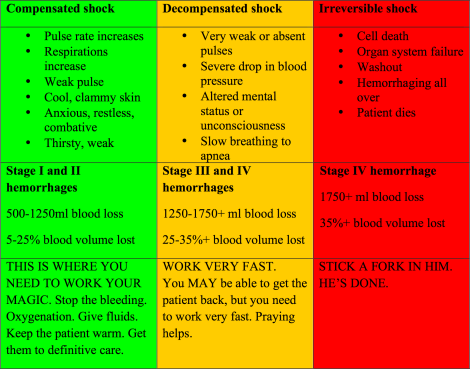
Hypovolemia is a low level of blood in your container from it springing a leak, hence the term “hypovolemic.” There are three stages in shock that you need to pay special attention to:
A quick note on blood pressure. Hypovolemic shock is usually defined as a symptomatic patient with a systolic blood pressure below 80 or 90mmHg. The key phrase is symptomatic patient. There are people, especially athletes, who can have resting heart rates in the fifties and blood pressures of 82/54mmg and they click along just fine. Don’t use blood pressure alone as a measurement for shock. It is one diagnostic tool in a toolbox. An array of signs and symptoms of shock need to manifest in various forms to guide your treatment.
Compensated shock: After someone is injured, you need to be very watchful for the signs and symptoms of compensated shock. In this stage, the body is compensating for the loss of blood occurring somewhere within the circulatory system. The body will constrict peripheral blood vessels to shunt blood to the torso and head in order to keep the main organ systems perfused. The patient’s heart rate will go up. Blood pressure will remain normal, and sometimes even increase slightly. Respirations will increase and sometimes increase in volume. He will become pale and cool and look freaked out. Some people want to fight, some people want to talk, some people start fidgeting around. In any case, you need to get it on here to prevent your patient from slip-sliding further down.
Treatment at this point is to stop bleeding wherever and however you can. If you have a tourniquet, use it. If not, direct pressure on pressure points and packing extremity wounds with hemostatic gauze and rolled gauze. If you have IV fluids, get a line (two is better, and try to have them with at least 18 gauge catheters) started and start getting saline or Lactated Ringer’s infused. If you have a BP cuff, you want to keep the systolic BP < or = to 90mmHg. The reason for this is that you want the body’s clotting mechanisms to go to work over whatever wounds there are. If a clot is forming over the broken vessel, a higher BP can blow the clot off and your patient will start bleeding to death again.
(H/T to SFMedic for this next section on Hextend. It is Gucci-level IV fluid and worth the coin, BUT – you better know how it works and how to use it, because it is not the same as Normal Saline or Lactated Ringer’s IV fluids.) If you maintain a radial pulse you will have roughly a 90mmHg systolic palpable B/P. If you lose the radial pulse give a small bolus 250 ml of Normal Saline, Lactated Ringer’s or ideally Hextend.
The reasons as mentioned, increased vascular pressure will stress any clot formation and restart bleeding which gets increasingly harder to stop as you deplete clotting factors and too much fluid dilutes what blood remains again making reclotting harder. For that reason a large molecule fluid like Hextend is preferred over the other fluids, because it uses oncotic pressure to pull fluid from the patient’s interstitial space into the vasculature, where it will stay for longer, helping keep blood pressures up. Normal Saline and Lactated Ringer’s more quickly leave the vasculature and make their way back into the interstitial space, which would lead to edema at the injury, impaired circulation and delayed wound healing.
If you have oxygen on hand, get it flowing. If you have a non-rebreather mask (NRB), 15 liters per minute (LPM) is recommended. A nasal cannula can be set 2-4 LPM. If you have to assist the patient with ventilations with a bag-valve mask (BVM), 15 LPM is the right setting as well.
Get the patient wrapped up in blankets and keep them warm. This is huge. People forget this a lot, and it is one of the most important things you can do.
Decompensated shock: This is an ominous change and does not portend for a very good outcome unless you are very aggressive in your resuscitation efforts. The patient’s BP will drop precipitously and his pulses will become very weak, even at the carotid and femoral arteries. If the pulses are fast, his heart is still trying to compensate by pumping blood faster, but there just isn’t enough blood. If the pulse is slow, his heart is shutting down because there isn’t enough blood to keep the heart muscle perfused. The patient’s mental status will deteriorate rapidly to unconsciousness. Breathing will become slower. Organ systems will start to fail. Blood becomes very acidotic and waste products from anaerobic metabolism begin to build up. This is a highly toxic state to the body. Decompensated shock does not last for very long and very quickly becomes irreversible shock.
Treatment for this is the same as compensated shock. If you have blood products around, they are going to work better than isotonic crystalloids like saline, but it may be too late already and you’d be better off using them on someone else.
Irreversible shock: This is fatal and there is nothing you can do for this patient except give them last rites. Cells die from lack of oxygen and break apart. The capillary layers open up and the patient starts bleeding from everywhere in a state known as washout, where lactic acid, CO2 in the form of carbonic acid, and coagulated red blood cells flood back into the circulatory system. The electrolyte balance in the body is upside down. Organ systems are now dead or dying. This person is dying.

The above famous picture of one of the victims of the Boston Bombing is a great example of what a person looks like in compensated shock. He has lost a lot of blood. He is very pale. And very importantly, look at the expression on his face. He looks kind of spaced out and detached. He’s not screaming in pain even though his legs have just been blown off. He’s just kind of hanging in there. This guy is definitely on the line between compensated and decompensated shock. Remember that look. If you ever see something similar to it, you have a very short time to work.
In hypovolemia caused by illnesses and exertion, the treatment is still the same. If the patient is conscious, alert, oriented, and able to swallow and keep down fluids, oral rehydration solution or similar can be given orally in addition to IV fluids to restore fluid volume and electrolytes.
Distributive shock
If hypovolemic shock is fluid draining out of the container, distributive shock, in a very simplistic form, is the container getting bigger while the amount of fluid stays the same, causing hypoperfusion from a lack of adequate blood pressure.
Your arteries and veins all have smooth muscle in them that dilates and constricts based on physiological parameters to keep you in homeostasis – i.e. perfused. Things like spinal cord injuries, brain injuries, anaphylaxis, sepsis, toxins, and medications can cause the smooth muscles to dilate severely, causing blood pressure to drop below a level that provides adequate perfusion.
In a spinal cord or brain injury, the dilation of the vessels will cause the skin to become warm, dry and flushed below the site of the injury. When the patient becomes hypoperfused because of this, he is said to be in neurogenic shock. So theoretically, you can have a patient that looks “shocky” at the head and face, but is warm, dry, and pink at the stomach and below. A key indicator of neurogenic shock is a low or normal heart rate, because the neural pathways that enable a sympathetic nervous system response – peripheral vasoconstriction and increased heart rate – have been disrupted.
In anaphylaxis, which is an extremely serious and lethal allergic reaction, the body reacts to an allergen by releasing massive amounts of histamine which causes systemic vasodilation which drops the blood pressure and raises the heart rate to compensate for the loss of pressure. Additionally, the patient’s upper airway swells rapidly and can become blocked. This is your primary concern, and we will discuss anaphylaxis in more depth on another post.
Sepsis is another serious condition that is caused by a systemic infection that results in systemic vasodilation from toxins released by pathogens in the body and blood. Patients with sepsis are usually ill to begin with and may have a compromised immune system, previous infection, or lack of healthcare as precursors to sepsis.
Treatment for all three of these types of distributive shock focus on getting the patient’s blood pressure back up to a perfusing pressure through aggressive fluid therapy. With anaphylaxis and sepsis, additional drug therapy will be used to treat the source of the problem causing shock. You will also give these patients oxygen and keep them warm.
The Triangle of Death
In shock, there is a thing known as the Triangle of Death. These are the three things that are absolutely, 100% sure to kill someone dead if they manifest.
- Coagulopathy: where the blood clotting / coagulation cascade stops
- Hypothermia: the patient’s core temperature drops
- Metabolic acidosis: lactic and carbonic acid flood the system
Now here’s the rub about resuscitation for shock.
A human’s pH level is normally around 7.35-7.45 on the pH scale of 0-14, with 0 being totally acidic and 14 being totally alkaline. Pure water at scientific room temperature of 25°C (approximately 77°F) has a perfectly neutral 7 on the pH scale.
The two isotonic crystalloids we use in the field for fluid resuscitation are 0.9% Normal Saline, which has a pH of 5.5, and Lactated Ringer’s (LR) solution, which has a pH of 6.5.
Secondly, both crystalloids are infused at room temperature, but our bodies run at 98.6°F.
So think about that for a minute. We are putting a cold, acidic solution into a patient that will die if he gets cold and acidotic.
To be fair, LR actually acts as a buffer and ultimately promotes alkalinity because it is transformed into bicarbonate AFTER it goes through the liver. However, it’s initially acidic when it goes into the venous system.
Hypothermia metrics in normal adults are as follows:
- Mild hypothermia: 90-95°F core body temperature
- Moderate hypothermia: 82-90°F core body temperature
- Severe hypothermia: <82°F core body temperature
This is something to think about when you are treating for shock. Consider warming fluids before administration and possibly using sodium bicarbonate if available.
The fact is, there’s nothing better to treat blood loss better than more blood, but you do what you can in the field.
[i] Bledsoe, Porter, Cherry, Paramedic Care Principles & Practice (Pearson Education, Inc. 2009) vol 1, p213.


Doc, It may be helpful to add to the compensated hypovolemic shock section this; If you maintain a radial pulse you will have roughly a 90 mmHg systolic palpable B/P. If you lose the radial pulse give a small bolus 250 ml of NS, LR or ideally Hexstend. Three reasons, as you mentioned, increased vascular pressure will stress any clot formation and restart bleeding which gets increasingly harder to stop as you deplete clotting factors and too much fluid dilutes what blood remains again making reclotting harder. For that reason a large molecule fluid like Hexstend is preferred over NS and LR as it is not third-spaced as NS and LR is and thereby maintains the fluid bolus itravascularly instead of interstitually which would lead to edema at the injury, impaired circulation and delayed wound healing.
The hypovolemic resuscitation protocols allow combat medics to leave their B/P cuffs, stethoscopes and tons of IV fluid at the FOB when they go on missions and just carry a couple of small bags of Hexstend.
I was trained in the ATLS trauma protocols as you were and when I first started learning this new “combat medicine” from the man who pioneered it, I couldn’t believe what I was hearing. I thought ” the AMA is going to burn us at the stake as witches and heretics.” After learning the science behind it and seeing it work on the battlefield I became a convert.
All your other work is impeccable.
LikeLike
When I certified TCCC, my mouth was agape at how efficient, brutally direct, and effective everything was. They must have had armed dudes guarding the doors to keep lawyers and suits from coming in while they wrote the protocols.
Thanks for the Hextend info. I’ll do some editing and get that in there.
Much appreciated and thanks for stopping by.
LikeLike
SFMedic, this is no longer taught in rigorous programs because it isn’t true.
The 90mm hg radial pulse point fallacy has been dis-supported by a fair number of studies over the past 5-7 years.
[if you have access to patients with Swan Ganz caths or other central venus pressure monitoring methods you can check this for your self]
The important thing is that if you have a radial pulse you [b]LIKELY[/b] have peripheral perfusion and this is a GOOD thing.
In resuscitative terms, our goal should be raising things one level, whether it’s one LOC level on the AVPU scale or one pulse point as found in assessment (Carotid–>femoral–>brachial/popliteal–>radial/pedal). Need to be careful we’re not either circulating pink koolade or blowing clots off of medium sized arteries.
LikeLike
I though I said ” you have roughly a 90 mmHg systolic pulse”
Who cares if its 85 or 91 exactly ? You are just rephrasing the points I made about pink koolade and busting clots. No one needs a Swan Ganz to know if they have perfusion compatible with life. But thanks for expanding the point about perfusion being the main goal.
The main point is to keep as many red blood cells circulating in the vasculature as possible to carry oxygen to the organs. You can’t do that with any IV fluid except blood and you can dramatically retard it with too much crystalloid or colloid fluid.
Whether you’re a grid-down survivalist or a Green Beret in the boonies, you need to learn to assess your patient and decide what he needs without all the fancy ICU equipment.
“Treat the Patient Not the Monitor”
LikeLike
Heh, we did have to have armed guards a few times but it wasn’t for the lawyers.
LikeLike
ZThis is an EXCELLENT primer for shock/hypoperfusion for the educable layman, ESPECIALLY as it is a no-fear intro to the whole shock cascade subject.
LOVE the triangle as a teaching tool.
LikeLike
Bluemud, I also teach guys how to do buddy transfusions in the field and even use untyped blood if they don’t know what their types are.
They key in emergencies with no other recourse is to watch the patient closely for hemolytic reaction and switch donors if it happens and the patient still needs blood. DOD thought they had discovered something new when this was first proposed, until we started getting calls from WW2 vets who said “Hell we was doing that in Europe and the Pacific in 1944.”
LikeLike
Start with the O pos donors that are common. stay away from A or B donors.
Donated my own blood to my patient in Iraq in 05
LikeLike
O NEG is the universal donor. O POS is indeed the most common type.
http://en.wikipedia.org/wiki/Blood_type
LikeLike
If you are fortunate enough have O neg available start there. thanks
LikeLike
Pingback: Anatomy & Physiology, Lesson 2.13: Taking blood pressure, without gear | Hogwarts School of Grid-Down Medicine and Wizardry·
In off grid medicine O2 seems to be first thing to get discarded due to wt and logistic burden, as well as low efficacy in making a difference in general trauma. I try to save it for HAPE/HACE or pulmonary injury. Just what I do.
At my definative off grid Tx facility I have a O2 concentrator on battery and solar power that is part of the drawover anesthesia set up.
I can be used for a Respiratory patient but is limited to 4 LPM.
LikeLike
Nice! As a pulm doctor that’s critical for me. I looked into oxygen concentrators, but they are very expensive. Cheapest I could find was here, and it’s still $400. No one in my tribe is on O2, so it’s not mission critical, but would be valuable if someone was doing off grid surgery.
LikeLike
CPAP and O2 potentially could be a big deal in managing respiratory complications of viral illness.
Poor mans low tech vent.
Both are low power enough to run on solar.
What are your thoughts? It’s your specialty. I’m always looking for input.
LikeLike
Viral, bacterial, inflammatory…the list goes on.
Found this:
http://www.secondwindcpap.com
that is an old RT selling used cpap or bipap machines for substantially less than new.
That and an old oxygen concentrator would go a long way.
In the old days they hand-ventilated patients using something very similar to an ambu bag. I’d think that would be difficult without lots of manpower.
The uninterrupted power supply would be difficult, and there is a limit to how much you can do with typical portable O2 concentrators. But you would save some folks, no doubt.
Will think on this further.
LikeLike
For long term bagging a patient put a foot operated zodiac pump on the circuit block the travel of the pump to prevent too much tidal volume. Set up with a reclining chair like a leg press machine at the gym.
LikeLike
Suggestion on CPAP units. Go for the noisy somewhat outdated ones that you can tune without worrying about the VERDAMNT CHIP!!!
Can’t adjust mine because every damn thing is on the chip. I haven’t YET tried to read the chip on my lap top but…
If yer working grid down or austere, you WILL want to tune it yourself.
(also think about what you might need for a nebulizer. Yes there ARE some antique manual glass DiVilbis ones around in a LOT of antique shops but you might want to think about the mechanics of the device (because even just water will help, and there are a couple herbals if I remember rightly that will also help. I’l get back to ya on which ones though Ephedra comes to mind even as a nebulized tincture).
LikeLike
A nebulizer can be set up with a foot pump as the air source and the cheap plastic neb can be cleaned and used many times.
A powerfull sanitizer solution for between use can be had from a MIOX pen.
(This spring MSR will release the se200 that produces larger quantities of mixed oxidizers)
Neb saline or water seems to help for secretion mobilization along with positioning and percussion.
LikeLike
For IV fluid resucitation in shock, I typicaly give 240cc bolus at a time only for signs of loss of perfusion to critical organs.
-LOC changes to include anxiety
-urine output is impractical in most austere situations
-a weak or absent radial pulse is a rough guide to adequate critical organ perfusion
I use positive pressure syringe delivered boluses as needed to get minimum perfusion restored.
My set up ideally is a large IV or IO cath, a lockable tail suficient to reach out of the bundle wrap around the patient, a 3 way stop cock, with a 30 or 60cc syringe, and a crystaloid / hexstend as available and as indicated. Draw fluid from the bag and then push to the patient by switching the stopcock.
When setting it up I first flip the bag and purge all air from the system out of the stop cock. This can be done at night by feel of fluid as well.
This system eliminates the hanging bag hazzard, keeps the bag warm with the patient (lines freeze in the arctic) , and prevents accidental infusion of too much fluid.
I typically will do one spiral wrap with the line on the forearm to secure the line to the patient.
In very cold climates I package a bag of fluids in carboard wrap with 1-2 MRE heaters in there as well. This pre warms the fluid just before use.
I have found that even a slight elevation of the feet makes a rapid short term bolus to the central venous pressure in the absence of a line or fluids but is not so practical for transport.
If you have other suggestions I would love to hear about it.
LikeLike
You sir, are on fire. Great tips. You have my wheels spinning re: my gear setup and techniques.
LikeLike
Very nice, practical suggestions. You also have my wheels turning.
LikeLike
pa4ortho, can you drop a line at headmaster_at_hogwarts@hotmail dot com?
Thx
LikeLike
Sound practice for those in the field to consider.
LikeLike
Pingback: Burns | Hogwarts School of Grid-Down Medicine and Wizardry·